Carers' Strategy
Carers in Barnsley
The care provided unpaid by the nation's carers is worth an estimated £132bn per year – more than the total spending on the NHS in England. In Barnsley, the value of such care is estimated to be around £605 million per year (Carers UK and the University of Sheffield (2015) ‘Valuing Carers 2015: the rising cost of carers’ support).
Many people across Barnsley spend lots of time providing unpaid care for a family member or friend who would be unable to cope without them. These people are referred to as unpaid carers or informal carers; they often say they are just being a husband, a wife, a mum, a dad, a son, a daughter, a brother or sister, a friend or a good neighbour.
For some people, taking on a caring role can be sudden and unexpected; someone in the family may have had an accident, or a child is born with a disability. For others, caring responsibilities can grow gradually over time; a family member may develop a long term physical or mental health problem, parents can't manage on their own, a partner or a child's mental or physical health worsens.
The amount and type of support that carers provide varies considerably. It can range from a few hours a week, such as picking up prescriptions, shopping and preparing meals, to providing emotional or personal care day and night, seven days a week.
What our carers survey told us
- Over 50% of our carers have been carrying out their role for five years or more, with 10% of those being in the role for 20 years or more.
- One in five carers told us they provide over 100 hours of care per week, with some describing it as a 24/7.
Being a carer can provoke a complex mix of emotions. It can be both rewarding and frustrating, and it can also be costly in terms of life chances, financial security and health and mental well-being. Carers play a vital role in the health and social care system. It’s widely acknowledged that they contribute significantly to making sure that the person they care for remains independent in their own home for longer.
Each carer’s experience is unique to their circumstances, and the care and support they provide can vary. However, carers share many similar experiences and challenges that impact the different aspects of their lives.
Our young carers’ needs are also included in all of the key priority areas of this strategy as there will be generic support needs, challenges and areas for change that will be just as relevant to a young carer as an adult carer. However, we acknowledge that there are also some differences in how we identify young carers and the types of support they require. Therefore, a specific priority for young carers has been included to focus on the outcomes that we want to achieve for young carers.
The carers within our community need to be recognised for the difficulties they experience, respected for all they are doing, and provided with information, advice, and support to continue providing good quality care whilst maintaining their own health and wellbeing.
Who is a carer?
Anyone can become a carer. Carers come from all walks of life, all cultures and can be of any age. For this strategy, the term ‘carer’ is used throughout the document and refers to individuals providing unpaid care to family members or friends.
In Barnsley, we define a carer as: ‘ordinary people whose lives have changed because they are looking after a family member, partner, or friend, who because of disability, illness, alcohol or drug use, a mental health condition or the effects of old age, cannot manage without help. The care they give is unpaid. This includes:
- Adult carers
Adults caring for adults over the age of 18. This includes adults caring for their adult children. Many carers have more than one caring responsibility; for example, carers could be caring for two family members, such as an elderly relative and a dependent child or a spouse. This is commonly referred to as 'sandwich or dual caring responsibilities' (Carers, UK 2019). - Former carers
Those who have stopped their caring role. This could be because of a change in the condition of the cared-for person. This includes the death of the cared-for person, the cared for person has recovered and no longer needs care and support, or the carer wanting/having to stop providing care. - Hidden carers
Hidden carers may not identify themselves as carers and may not seek support or information that would benefit them. They may also choose not to seek support and information about their caring role. - Mutual carers
Those who require care and support that are also providing care and support (interdependent caring). - Parent carers
A parent carer provides care for a child with additional needs (under the age of 18) and have parental responsibility for the child. - Working carers
Working carers combine caring for another person with working. Supporting carers to remain in work can bring considerable benefits to carers themselves, employers, and the wider economy. - Young carers
Young carers are children and young people under the age of 18 who look after someone in their family who has an illness, disability, is affected by mental ill-health or problematic use of alcohol and/or drugs. They take on the practical and emotional caring responsibilities that would normally be expected of an adult. - Young adult carers
Young people aged between 18 and 25 who are caring either for another child or young person, or an adult.
Within each of the groups listed above, some carers have a 'lifetime' of caring due to the nature of the cared-for person's needs (eg those who care for individuals with autism, with learning disabilities, with significant mental health conditions developed in childhood or early adulthood). These carers often provide a substantial number of hours of care and support a week.
Equality and diversity
We also recognise that carers in Barnsley are diverse and come from a range of different cultures, backgrounds, and communities, such as but not limited to, the armed forces, black, Asian and ethnic minorities, lesbian, gay, bisexual and transgender (LGBT+).
We acknowledge that some carers will need to be reached and engaged in various ways and may require different types of support. Our equality impact assessment and action plan will make sure that all carers receive information and advice relevant to them, have equal opportunities to access services, and that barriers are identified and addressed so no one is excluded or disadvantaged.
Our vision, aims and key priorities
Our vision
Carers are identified and recognised and have access to information and practical and emotional support to help them achieve the outcomes which matter most to them.
Our aims
More carers in our community will:
- Be recognised and identified as a carer at the earliest opportunity, so they receive the appropriate information and advice for them, their family, and the person they care for.
- Understand their rights as a carer and have access to an assessment, so they receive support and sufficient breaks to look after their health and mental well-being.
- Be enabled to have a life outside of their caring role and also be supported to work or undertake training and education opportunities.
Overview of key priorities
This strategy sets out our partnership approach for working together and supporting our carers across the following seven key areas.
- Raising awareness to increase the identification of carers
- Working with carers
- Assessing carers needs
- Carers health and wellbeing
- Carer breaks
- Helping carers stay in work
- Young carers
- Parent carers
Stakeholder and carer engagement
While there are services and support options available to carers in Barnsley, we recognise that there are gaps and areas that require improvement or further development. Therefore, we need to continually work together to improve outcomes for our carers.
This strategy has been developed with a range of stakeholders, including carers and the Carers Forum, to ensure that views and expertise from across the borough have helped shape the strategy’s key priorities for the next five years.
To identify our key priority areas, we have consulted with carers and stakeholders through a range of methods:
- face-to-face consultation event
- verbal feedback via Teams meetings
- questionnaire feedback, gathering views and experiences on a range of topics, including:
- the four national action plan themes
- services and systems that work for carers
- employment and financial wellbeing
- supporting young carers
- recognising and supporting carers in the wider community and society
- ADASS (Association of Directors of Adult Social Care) Carer Quality Markers Self-Assessment Toolkit, completed in consultation with carers and key stakeholders
- interviews with carers that have had a carers assessment via adult social care
- face-to-face focus groups with the Carers Forum
- public carers survey*.
- feedback from carers attending the DISC (Dementia Information and Support Course) training courses
- survey with service users and staff from the Barnsley Carers Support Service*
- learning from coronavirus pandemic (stakeholder meeting and carer survey)
- consultation events and focus groups with young carers and the Young Carers Council
- feedback from various delivery groups and strategic boards
- consultation survey on the proposed priorities of the strategy
- work with the Barnsley SEND Parent and Carers Alliance is underway to ensure they're involved in the further development of the strategy and action plan
* It should be noted that survey respondents are not representative of all carers in the Barnsley area, but the results give an indication of the demographics and needs of this group.
From the stakeholder engagement and consultations that have taken place, we acknowledge the need to reach and engage with more carers to obtain a wider representation and perspective of their needs.
National and local policy
National policies have a significant impact on the approach to how carers are supported.
Several local strategies and plans, also have aligned priorities and involvement from a number of the key partners.
National strategies and policies
The following national strategies and policies all have a significant impact on the approach to how carers are supported. They acknowledge the important contribution carers make and place them on the same footing as the person they care for when it comes to accessing services and support.
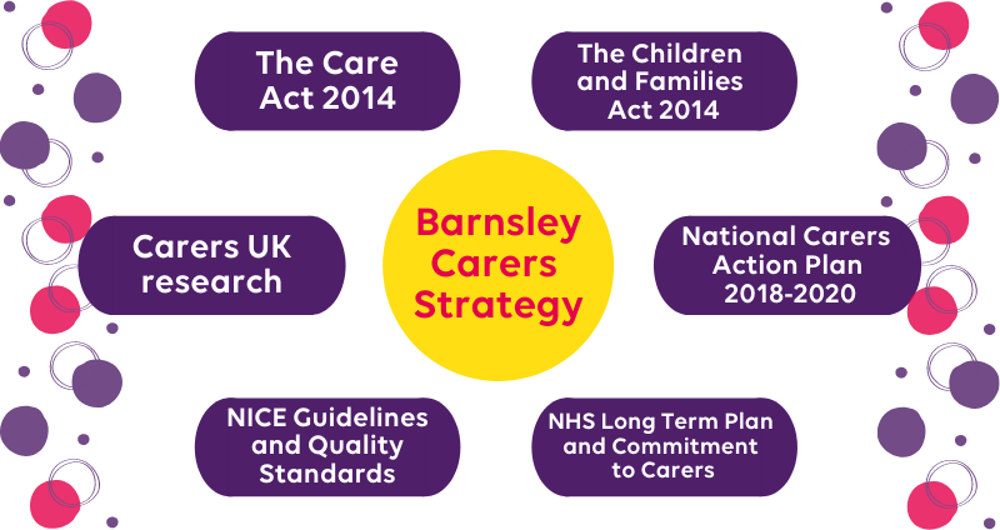
- The Care Act 2014
- The Children and Families Act 2014
- The national Carers Action Plan 2018-2020
- NHS Long Term Plan 2019 / NHS Commitment to Carers (2014)
- NICE Guidelines and Quality Standards
- Carers UK research
While the strategy builds on these policies, it places a strong focus on the NICE (National Institute for Health and Care Excellence) Supporting Adult Carers Quality Standards (NICE Supporting Adult Carers Quality Standards 2021). We feel that these statements pay particular attention to the carer journey and will enable us to focus on the key touch points where carers tell us they face challenges and change is needed.
Local strategies and policies
The Carers' Strategy and our wider work with carers is closely linked to several local strategies and plans, all of which have aligned priorities and involvement from a number of the key partners.
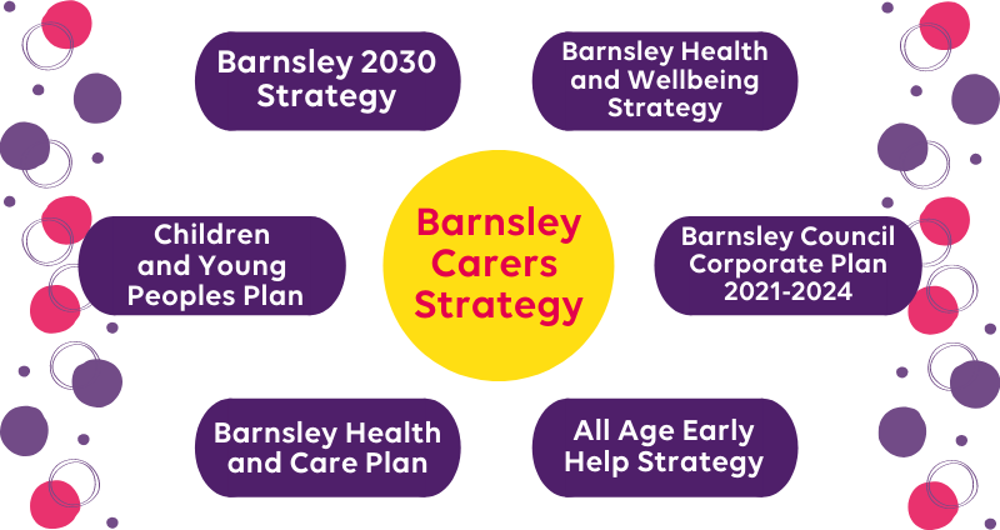
- Barnsley 2030 strategy
- Barnsley Health and Wellbeing Strategy
- Barnsley Council Corporate Plan 2021-2024
- All Age Early Help Strategy
- Barnsley Health and Care Plan
- Children and Young People Plan
Other relevant documents that the Barnsley Carers Strategy link to include:
- Barnsley Mental Health Strategy
- Children and Young People’s SEND (Special Educational Needs and Disability) Plan
- Preparation for Adulthood Strategy
- Joint Strategic Needs Assessment
- Stronger Communities Partnership Plan
- Safeguarding Adult and Children’s Strategic Plans
- Public Health Strategy
- Learning Disability Plan
- Dementia Action Plan
- British Legion Report - Unpaid Carers in the Armed Forces Community
Barnsley carers
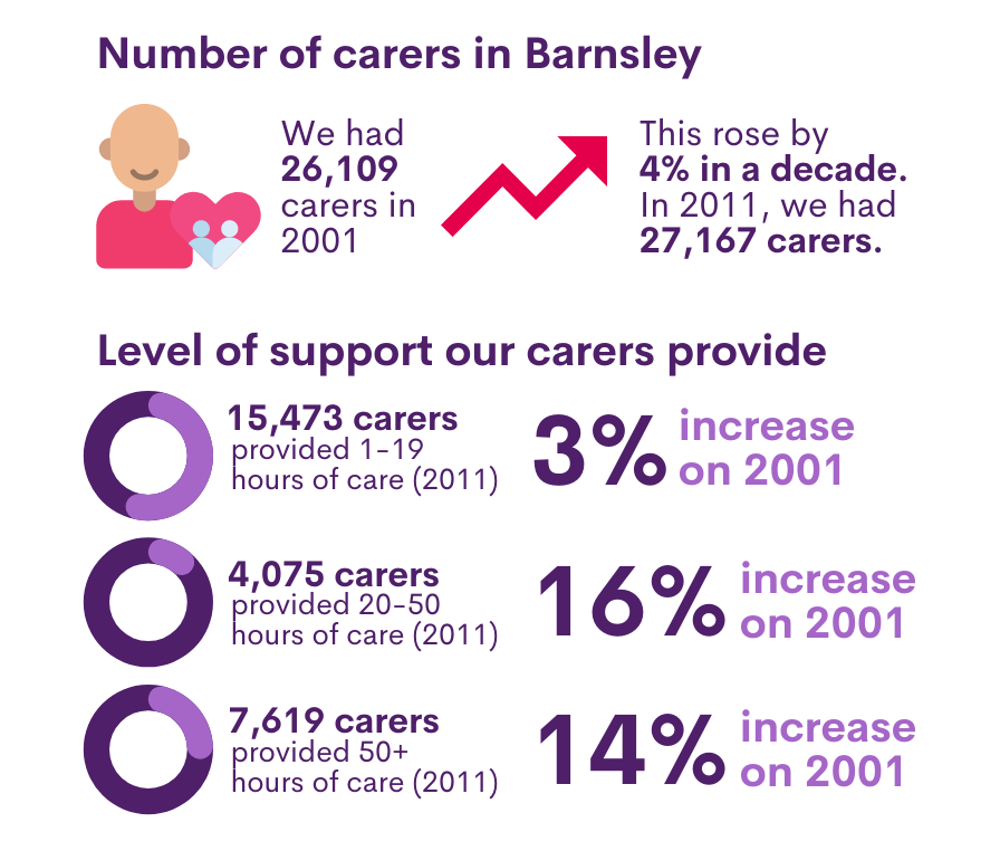
The number of unpaid carers recorded in Barnsley by the 2011 census was 27,167.
This was equivalent to approximately 12% of the population of the borough.
Prevalence of carers in Barnsley
By 2015, a national research study stated that the number of carers in Barnsley had increased by 4.6% to 28,429 (Valuing Carers 2015 - the rising value of carers’ support, Lisa Buckner University of Leeds, Sue Yeandle University of Sheffield). By 2037, Carers UK have calculated that the number of carers in the UK will increase by 40%, meaning we would have approximately 39,800 carers in Barnsley.
The number of carers recorded in Barnsley at the time of the 2011 census and a breakdown of the level of care that they provide is below:
- Total number of carers in 2001: 26,109
- Total number of carers in 2011: 27,167
- Numerical rise in a decade: 1058
- Percentage increase: 4%
- Carers providing 1 to 19 hours of care (2011): 15,473 (3% increase on 2001)
- Carers providing 20 to 50 hours of care (2011): 4075 (16% increase on 2001)
- Carers providing 50+ hours of care (2011): 7619 (14% increase on 2001)
While a large percentage of the carer population remains hidden in Barnsley, approximately 12,745 adult carers are known to or registered with the following services:
| Name of service | Number of carers known to them |
|---|---|
| Adult Social Care via Care Act Carers Assessments (2020/21) | 1921 (single assessment: 414 and joint assessment: 1507) |
| Carers registered with GP practices (as of May 2021) | 8765 |
| Barnsley Carers Support Service (1 August 2018 to 31 March 2021) | 1892 |
| Beacon South Yorkshire (2019/2020) | 167 |
Please note: double counting may occur in the above numbers.
This is 46.9% of the estimated number recorded by the census 2011.
In addition, the 2011 census data also reported that Barnsley has 453 carers aged under 16, with 354 providing care for under 20 hours per week, 52 over 20 hours, and 47 over 50 hours per week. There are also 1482 carers aged 16 to 24, with 1018 providing care for under 20 hours per week, 249 over 20 hours, and 215 over 50 hours per week.
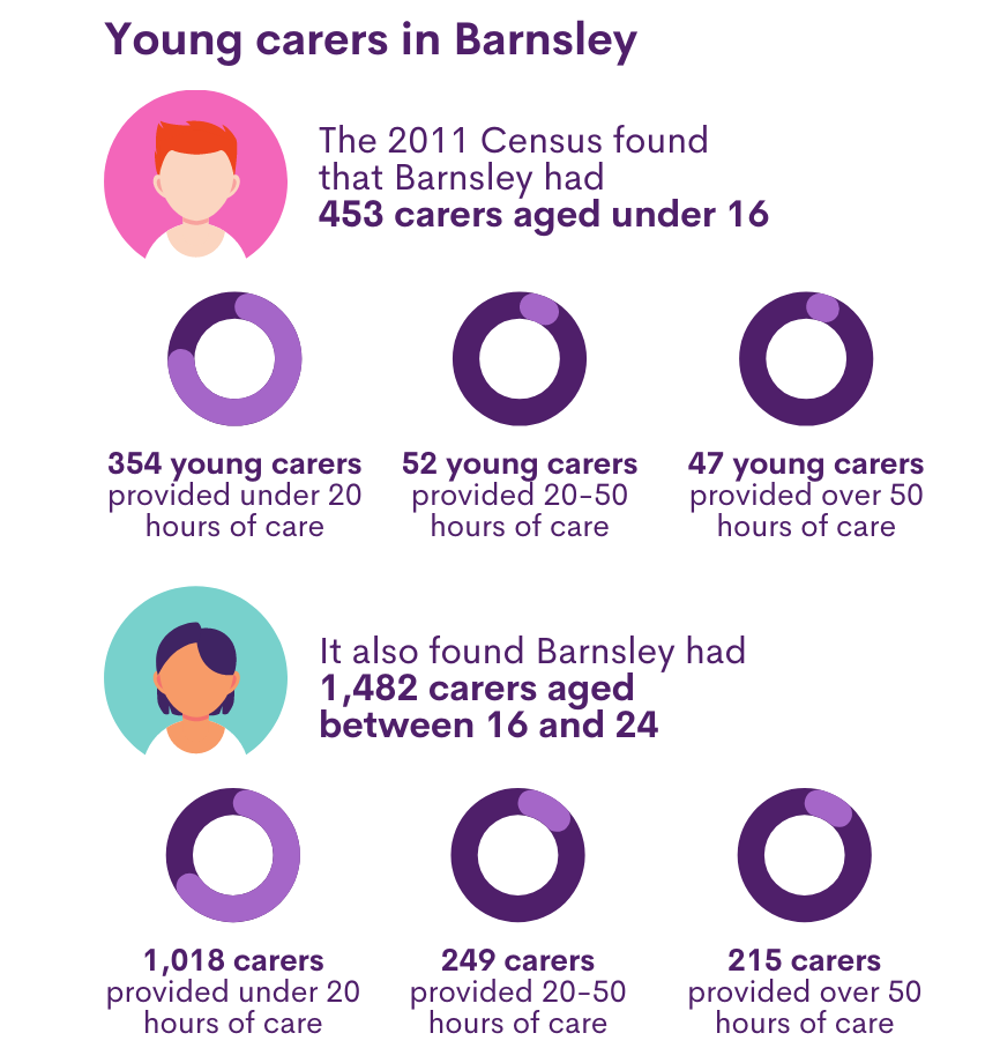
The Young Carers service, delivered by Barnardo’s, is commissioned to work with 100 individuals every year – with 30 young carers accessing the service as of quarter two of 2021/2022.
How do we compare to the national picture?
Carers UK states that one in six adults are providing unpaid care, equating to 8.8 million unpaid carers nationally (Carers UK Research Summary from Carers Week 2019). The number of people aged 65 and over who are caring has grown from 1.4 million to over 2 million.
Carers UK estimate that, nationally, 58% of carers are female and 42% are male. In Barnsley this would equate to 15,757 women and 11,410 men, although we know that 75% of the carers accessing the Barnsley Carers Service are female.
In 2020, research estimated that 7144 people in Barnsley over the age of 65 provide unpaid care to a partner, family member or other person. Of these, 3378 provide more than 50 hours of unpaid care each week (POPPI, Projecting Older People Population Information System, 2021).
Of the 8,765 individuals registered as a carer by GP practices, 52% are aged over 65 years. We know from our survey of the Barnsley Carers Service users that all respondents identified as being white, over 85% were female and the majority (66%) were aged between 40 and 70 years old.
The 2019 GP Patient Survey found that carers are more likely to report having a long-term condition, disability or illness than non-carers – 63% of carers compared with 51% of non-carers. In Barnsley, this would equate to 17,155 carers of the estimated 27,167 carers in the borough.
The 2011 census also identified 177,918 young carers in England and Wales, with one in eight of those being under eight years of age. This is believed to be the tip of the iceberg, with some estimates suggesting that as many as one in five schoolchildren are young carers (University of Nottingham 2018), with this number increasing during the COVID-19 pandemic.
Further information regarding carers in Barnsley is included in Appendix A.
Caring during the COVID-19 pandemic
Carers UK estimated that carers in the UK delivered on average 25 additional hours a week of unpaid care whilst COVID restrictions were in place. The social, physical and emotional impact of this has been huge and cannot be overlooked as this is still being felt by many families. The virus disproportionately affects older people, those with disabilities and/or long-term health conditions - resulting in both the numbers of carers - and the level of caring provided - increasing. Carers UK advise that 70% of carers now provide an average of ten extra hours of care and support a week.
Caring for someone, whilst often be rewarding, is also challenging under normal circumstances. However, the COVID-19 pandemic has added additional pressures to informal carers, impacting not only on their physical health and mental wellbeing but also those they are caring for. The added pressures include increased social isolation, an increase in hours of care being provided (often 24/7) with no breaks, a reduction in some support, particularly face-to-face appointments, and the suspension of day-care services.
“We are not out of the woods yet; we fear another lockdown and a suspension of services again. We don’t want to be housebound again. We don’t want to feel trapped”.
Of the respondents completing our carer survey
- 64% highlighted that they felt that COVID-19 had increased their caring responsibilities - “Self-isolating meant no external respite”.
- Over 70% stated that the pandemic had affected their mental well-being and led them to worry more about the person they are caring for. Over 30% felt unsupported in their caring role. Only 11% felt their mental wellbeing had been unaffected by the pandemic.
- In relation to whether the pandemic had affected their physical health, over 50% of respondents said that this hadn’t but, 24% felt that this had affected them physically.
- 65% stated that they felt the pandemic had not affected their ability to be a carer but 33% felt that this had.
- "When he’s alright, I’m alright, but those lockdowns were harsh. Everything stopped; all our routines and social trips out just stopped. I know they had to. It was hard to keep him entertained, but what could I do? I just had to get on with it. At times I felt trapped. I still do even though things are opening. He is not the same as he was before lockdown."
Young carers fed back what impact they had felt from the pandemic
- Some young carers said they felt under pressure in the community when out shopping or doing other activities during the lockdown. Some needed to accompany their cared-for person to activities such as hospital appointments. They felt they had been questioned about their role and the validity of their presence.
- “I have been asked for proof that I am a carer for my mum; this has been difficult as I don’t want to have to share private information with shop workers. I felt judged, and that assumptions had been made about me and my family”.
- “It’s stressful shopping for my own family and elderly grandfather who needs to shield. I go to the small local supermarket at least three to five times a week. It’s hard to carry shopping back. Sometimes I take my younger sister to help carry items or take mum’s mobility scooter.”
- Young Carers also reported that not being at school as much gave them a sense of relief as they could be with their cared-for person more, and this relieved some of the anxiety and concern they felt when they had to go to school.
The priority areas of the strategy will consider the challenges that carers have faced during the pandemic. As we ease out of lockdown and rebuild our support networks, we need to ensure that we do all we can to identify our carers, so they can access information, advice and both practical and emotional support.
Our priorities and next steps
Our Carers' Strategy sets out our partnership approach to work together and support carers across six key areas.
No single organisation can deliver the changes required alone; the strategy sets out a partnership approach for working together to support carers.
Our priorities
In developing the strategy we have compared what our local carers tell us to what carers say nationally, and there are many common themes reflected in the priorities identified.
This webpage sets out our partnership approach to work together and support our carers, and through this strategy we'll achieve the following:
- Priority 1 – Raising awareness and increasing the identification of carers: Raising awareness so that more carers are identified and encouraged to recognise their role and rights as a carer by health and social care organisations, schools and colleges, voluntary sector services, community groups and private businesses.
- Priority 2 – Working with carers: More carers are supported to participate in decision making and care planning for the person they care for.
- Priority 3 – Assessing carer's needs: More carers have a carers assessment and have the opportunity to discuss what matters most to them, including their health and wellbeing, social care needs, financial support, work, education or training.
-
Priority 4 - Carer's health and wellbeing: Provide information, advice and support to carers to help them manage their own health and wellbeing to remain as physically and emotionally well as possible.
- Priority 5 – Carer's breaks: Carers are given the opportunity to discuss the value of having a break from caring and the flexible options that are available to them to access.
- Priority 6 – Helping carers stay in work: Carers are offered supportive working arrangements by workplaces.
- Priority 7 – Young carers: Support young carers to prevent inappropriate caring and provide the support they need to help them balance their caring role with their rights to be children/young people.
- Priority 8 – Parent carers: Work is currently taking place with the Barnsley SEND Parent and Carers Alliance to co-produce this priority.
Appendix B gives more detailed information about each of the priorities.
The strategy will also help inform the re-commissioning of the Barnsley Adult Carers Service and the Young Carers Service and will help guide decisions on the service delivery models to contribute to the above priorities.
Carers Strategy Delivery Plan
This strategy sets out a partnership approach for working together and supporting our carers across seven key outcome areas. No one organisation can deliver these outcomes and the changes that are required alone.
A comprehensive delivery plan will be developed by the Carers Strategy Steering Group, Carers Forum, Barnsley SEND Parent and Carers Alliance, and the Young Carers Council which will provide detail about what we'll do to meet the aims of the strategy and our eight priorities. The plan will include timescales and accountability for leading on specific actions and measures to assess progress and achievement.
The delivery plan will identify key actions and outcomes for each year. We will achieve these actions, which over time, will allow us to build on and deliver the priority outcomes outlined in this document.
Governance and review
It’s important for us to understand if we are on track to achieve our ambitions and outcomes for carers in Barnsley.
Over the lifetime of this strategy, the steering group will work closely with the key delivery groups, partnership boards across the borough, the Carers Forum, Barnsley SEND Parent and Carers Alliance and the Young Carers Council to report the activity and progress of the action plan and seek support to address any challenges and barriers that are identified.
Monitoring activity will take place on both a quarterly and annual basis and we will publish an annual report which will be made available on the council website. This will also allow us to assess whether our aims and priority areas remain relevant. Progress updates will also be shared on social media as part of the communication plan.
Gathering continuous feedback from carers will be an essential part of the monitoring and continuous development process.
How we'll know if we're making a difference to carers
We'll monitor our progress using the key indicators from the Survey of Adult Carers in England and the National Outcome Frameworks.
We'll also use outcomes collected by the adult carers and young carers service.
Measuring success
We will monitor our progress using the key indicators and measures from the Survey of Adult Carers in England and the National Outcome Frameworks. We will also use outcomes collected by the Barnsley Adult Carers Service and the Young Carers Service.
This will capture feedback on topics that are indicative of a balanced life alongside an unpaid caring role:
Public Health Outcome Framework
- B18b - Social isolation: percentage of adult carers who have as much social contact as they would like (18+ years).
Adult Social Care Outcomes Framework
- 1d - Carer-reported-quality-of-life-score
- 1i - Proportion of service users and carers who reported that they had as much social contact as they would like
- 3d - Proportion of service users and carers who find it easy to find information about services
NHS Outcomes Framework
- 2.4 - Health-related quality of life for carers
A local performance dashboard will be developed to measure progress and achievement against a range of core activity indicators and outcomes aligned to the strategy’s priorities.
Annual survey
We will work with carers to design and develop a public survey based on the key outcome areas of the strategy and national Survey of Adult Carers in England so we can also capture the views of carers who do not access support from health and social care.
We will begin work on the survey when the strategy is implemented to give us a baseline position and will be repeated on an annual basis to measure progress across the lifetime of the strategy.
Appendix A
Facts and figures from national and local research.
Carer facts and figures
- Over 50% of our carers have been carrying out their role for five years or more, with 10% of those being in the role for 20 years or more.
- One in five carers told us they provide over 100 hours of care per week, with some describing it as a 24/7 role.
- 45 percent of carers told us they live with a disability or a long term condition, with 24% indicating a mental health problem or illness.
- 27% of our carers told us they were employed full time and 24% told us they were not in paid work.
- 40% of our carers look after a parent, followed by 27% looking after a partner and 21% looking after a child.
- 63% of our carers told us that they are the sole carer for the person or people they care for.
When asked about the people our carers support:
- 51% have a longstanding illness
- 45% have a physical impairment
- 28% have problems connected to ageing
- 25% have a sensory impairment
- There are at least 1300 families in Barnsley living with a child or young person with special educational needs (SEND). Carers in the SEND community need extra support.
- In quarter 2 of 2021/2022, 30 young carers were accessing support through the Young Carers Service, 87% of these individuals were under the age of 12, and 13% carers were aged between 12 and 17 years of age. Of these carers aged under 17, 23 (77%) were female and seven (23%) were male.
The wider picture
- Research undertaken by Carers UK nationally found that women have a 50:50 chance of providing care by the time they are 59, compared with men who have the same chance by the time they are 75 years old. Women are also more likely to be sandwich carers (combining caring for elderly relatives with work and childcare).
- The gender imbalance reduces amongst older carers; the gender split is 50:50 of carers aged between 75 and 84. Carers over 85 are more likely to be male (59%) than female (41%) – many caring for their partners.
- Royal British Legion research has shown that working-age members of the ex-service community are more likely than the adult population of England and Wales to have caring responsibilities. 23% compared to 12% in the 16-64 age group nationally. This is equivalent to around 990,000 people.
We acknowledge that the data available regarding carers, particularly young carers, is limited and the demographic information is mostly from our adult commissioned service and carers survey. There is a need to work together and share data and intelligence so we can better understand the profile of our carer population and their needs to assist in the planning of support provision.
Appendix B
The seven priorities we'll aim to achieve through this strategy.
Priority 1 - Raising awareness and increasing the identification of carers
More carers are identified and encouraged to recognise their role and rights as a carer by health and social care organisations, schools and colleges, voluntary sector services, community groups and private organisations.
A key barrier to the access of appropriate support to carers is that they are often not identified. Identifying carers is often a challenge as many people do not see themselves as carers. According to research undertaken by Carers UK, 54% of carers took over a year to recognise their caring role and 24% took over five years.
While being a carer doesn’t define a person, it may mean that they have legal rights including the right to certain types of financial support, practical help, assistance technology and rights in the workplace.
Through the strategy we aim to raise the profile of carers in the borough to support residents to recognise themselves as a carer at the earliest possible stage in their caring journey.
Our partners in health and primary care will be instrumental in the delivery of this priority. This is underlined by NHS England’s Commitment to Carers (2014) which states that ‘70% of carers come into contact with health professionals, yet health professionals only identify one in ten carers with GPs, more specifically, only identifying 7%.
Work also needs to continue within education, health and social care to support the identification of young carers. Young carers often feel reluctant to be identified due to concerns over possible social care involvement and the general stigma of being a young carer.
While being a carer doesn’t define a person, it may mean that they have legal rights including the right to certain types of financial support, practical help, assistance technology and rights in the workplace.
What engagement with carers and stakeholders told us
- There is a lack of awareness of who a carer is. “I feel invisible.”
- Carers are usually identified too late when they have already reached a crisis or emergency.
- Carers feel that they are not recognised by professionals across a wide range of services.
- Carers who participated in the British Legion’s research of unpaid carers in the armed forces said they felt insufficiently supported by relevant services and “wouldn’t know where to look for support as a carer” (Unpaid Carers in the Armed Forces community).
- 12,745 adult carers have been identified in Barnsley – this is 46.9% of the number of carers recorded by the 2011 census.
- We feel that we are not always told what our rights and entitlements are, particularly around benefits. 45% of those responding to the Carers' Survey said that they had experienced financial difficulties due to their caring responsibilities.
- There needs to be clear guidance on recognising carers including their roles, rights and responsibilities to then enable the correct pathway to follow once a carer is identified.
- 49% of carers responding to the Carers' Survey found it fairly or very difficult to find information and advice about support services or benefits to help them.
- The information and support available for carers should be promoted through a variety of different communication methods.
- The entitlement of services and support offer across adult and children’s services differ due to different policy and legislation. This information needs to be made clear so carers are aware of what support is available and how they can access this when making the transition between services.
What we aim to do
- Develop a multi-agency communication plan to raise the profile of carers and help residents to identify themselves as carers. The plan will also consider the different types of carers in the borough, so information is targeted and appropriate for the intended audience.
- Raise awareness of caring and the role of unpaid carers through regular public awareness campaigns including National Carers Week and Carers' Rights Day.
- Co-produce a Carers’ Charter highlighting a key set of commitments that carers can access in order to understand what they can expect from organisations.
- Increase identification and support through primary care and work with our partners to implement the NHSE (National Health Service England) GP Quality Markers for carer-friendly GP practices.
- Ensure carers are able to receive good quality information and advice which does not contain professional terminology.
- As part of the NHS Commitment to Carers explore implementing the Carer Passport Scheme across the borough using learning from our partner, SWYPFT (South West Yorkshire Partnership NHS Foundation Trust).
- Co-design a training package that can be delivered to services and professionals to help them recognise carers and know where to signpost them.
- Explore ways to support carers to gain IT and digital skills. This will mean that carers are better able to stay connected and access information and advice.
Priority 2 – Working with carers
More carers are supported to participate in decision making and care planning for the person they care for.
Carers can share valuable knowledge about the person they care for and are often key to understanding the person's needs and preferences which can help practitioners provide the right care and support.
Carer’s value being recognised and respected as core members of the team around the person they care for. Providing the person gives consent and their wishes remain central, carers should be supported to actively participate in decision making and care planning for the person they care for. This will help to ensure that care planning is based on accurate and detailed information, as well as supporting the carer in their role and helping to sustain the caring arrangement.
What engagement with carers and stakeholders told us
- Carers feel that they are not always involved or listened to in decision making and care planning across health and social care. “Respect, involve and treat me as an expert in care.”
- Carers are not always involved in or do not fully understand the discharge process from hospital. “There are so many examples of people being discharged from hospital without sufficient mental health after care and carers are amongst this group. I attempted suicide and when I was discharged all I wanted was a phone call each day to check that I was alright, but that could not be organised by the hospital discharge team”.
- Healthcare professionals appear unaware of the carers support available and so rarely signpost carers to sources of information or support.
- Information sharing/consent is a constant barrier. “All too often I am ignored or told nothing due to confidentiality and yet I am the one who looks after him.”
- Include emergency/contingency plans for crisis situations in care support plans, set out the assessed needs and what arrangements have been agreed so the cared for person is safe should any unexpected situation or emergency happen.
- Next steps and plans need to be shared with the carer and reviewed on a regular basis. “If support is right for the cared for person then it will make it easier for me.”
- Better partnership working between services is needed to avoid duplication of work and improve referral and care pathways – carers and the people they care for need access to support in a timely manner.
- Better links are needed between adult and children’s services.
- Better transitional arrangements are needed for young carers who will transition into becoming an adult carer or parent carers who will similarly transition into caring roles for their adult child.
- Carers often find it difficult navigating around the system and understanding the terminology used by professionals and which services deliver what.
- Carers would like training around health conditions of the people they look after to support with their caring role.
What we aim to do
- Review care planning procedures and embed carer involvement into the process and working practices.
- Work with health and social care professionals and services to ensure that they seek consent from the cared for person to share information about their care and support with their carer, and when consent is provided that the carers’ knowledge and expertise is considered when developing care and support plans for the cared for person.
- Within the above consideration information sharing agreements will be explored to look at how information can be shared between health and social care, to reduce the need for the cared for person and carers repeating information.
- Review referral and care pathways between services aiming to make these easier to use and understand, minimising the stress caused to carers trying to navigate the system.
- The Adult and Young Carers Services will work with partner agencies and:
- work with carers to co-design and deliver a training programme for education, health and social care professionals to better understand the role of carers and young adult carers in providing care and support to the cared for person to encourage involvement.
- co-design and implement a training programme for carers, prioritising the areas advised by carers themselves, as beneficial including training around health conditions of the people they look after.
Within this priority we will improve how we reach and engage with more carers across the borough so they have an active voice and can contribute to the development and improvements of local services for themselves and the person they care for. “We want action, not words”.
We will continue to support and/or work with the Carers' Forum, Barnsley Send Parent and Carers Alliance and the Young Carers Council so that carers have an active voice in helping to improve the quality of support and services in the borough. Within this, we'll work with a range of organisations, community groups and forums to ensure carers from a range of backgrounds and groups are identified and have a voice.
Priority 3– Assessing carer's needs
More carers have a carer's assessment and are given the opportunity to discuss what matters most to them, including their own health, wellbeing and social care needs, work, education or training.
Caring can be a hugely rewarding experience but carers often find it challenging to look after their own health and wellbeing. Caring can impact all aspects of a person’s life, from relationships and health, to finances and work. Caring without adequate information, advice and support can have significant consequences for both the carer and the cared for person.
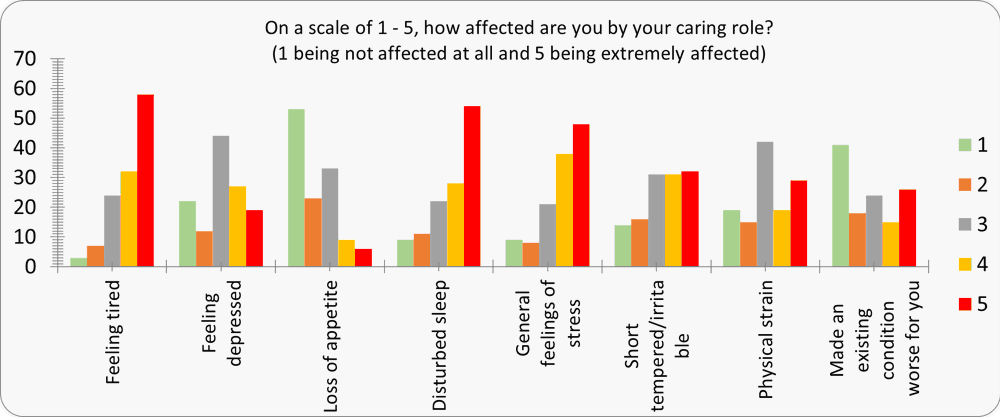
20% of people responding to our Carers' Survey highlighted that they had felt extremely affected by tiredness, disturbed sleep, general feelings of stress, under physical strain, short tempered and had felt an existing condition worsen.
We must not under-estimate the impact of caring on a carer’s mental health. “Carers need to be given priority to receive person centred and timely mental health support, when they need it, so that they can continue in their role."
A carer's assessment should focus on what matters most to the carer and what will help them so they can be better supported in their caring role. It is important that service providers who carry out assessments (both Care Act assessments and non-Care Act assessments) focus on the carer as well as the person they care for, considering how their caring role affects their overall quality of life including their health and wellbeing and emergency planning.
We want more carers to have access to an assessment at the earliest opportunity, receiving the most appropriate support to manage their caring role and achieve the outcomes which matter most to them in their lives. To help with this, we want to have better quality conversations with carers, which discuss the things which matter most to them, and deliver information and support which helps them to achieve their personal outcomes.
What engagement with carers and stakeholders told us
- Assessments often focus on the cared for person rather than the carer themselves, particularly if a joint assessment is undertaken. “I was never asked how I was. I was asked to leave the room whilst my husband with dementia was assessed. They listened to his answers even though he doesn’t believe he has dementia or that we have any problems, but they didn’t listen to me.”
- Carers are often told that unless the person they care for is assessed by adult social care they cannot access a carer's assessment.
- When a joint assessment is carried out ensure carers can speak openly and freely about their caring role and if not offer them a single assessment.
- Allow carers voice to be heard in relation to their rights and what support they would like.
- When assessments take place carers would like to discuss the options around respite. Carers tell us they need flexible respite to enable them to attend their own health and other appointments.
- Carers would like assistance in understanding and completing paperwork and forms. “It’s not easy filling forms in, everything is electronic. It’s good to have someone helping me to do this so that I can explain our situation. I was rejected for Attendance Allowance the first time I applied, then I got help to appeal, but this all took time."
- Carers tell us they often have to repeat their story when they access different services.
- Of the carers interviewed who have had a carer's assessment the majority said that they value the support they receive from social workers.
- Carers tell us that within the SEND community there is a fear of children being taken away and this limits involvement with social workers. This may account for lower numbers of carer assessments from parent carers. Few complain about services, for fear of children being taken away.
What we aim to do
- Complete the thematic audit of adult social care’s approach to carers and use the findings to facilitate improvement and/or change to the assessment process in relation to the Care Act.
- Work with other service providers to ensure that staff who carry out carer's assessments have the necessary training and skills to carry out the role.
- Review the emergency planning process and ensure all carer's assessments include an emergency plan and that services are joined up to respond if required.
- Undertake a mapping exercise to identify what support is available, where there are gaps in provision and how referral and care pathways work between services with a view to developing a single carer pathway and improve joint working between services.
- Review and develop information sharing agreements to enable better joint working between agencies and so that carers don't have to share the same information several times with professionals.
Priority 4 - Carers health and mental wellbeing
Provide information, advice and support to carers to help them manage their own health and wellbeing to remain as physically and emotionally well as possible.
Health and wellbeing
While caring can be very rewarding and fulfilling it can also be draining and exhausting and have a considerable negative impact on a carer’s mental and physical health and wellbeing. If carers, regardless of their level of caring, are not supported to look after their own physical, mental, and emotional wellbeing, then their ability to maintain their caring role is also at risk.
Unsurprisingly, carers who care for more than 50 hours a week, and carers who have been caring for over 15 years, are more likely to report poorer health. This may be especially true for parental carers of children with disabilities, as this can mean a lifetime of caring; and also, for older carers, as they are much more likely to have a long-term health condition of their own.
Carers are seven times more likely to say they are always or often lonely and feel isolated compared to the general population.
What engagement with carers and stakeholders told us
- Carers tell us that their caring role triggers a range of emotional feelings and anxiety “Your world gets smaller and smaller, I feel trapped. I feel cheated that I haven't got the life I planned, then I feel guilty for thinking this way".
- More emotional support is required and in a timely manner – being met with a waiting list is not good enough.
- 45% of our carer responding to our carers survey highlighted that they live with some form of disability and/or long-term condition themselves. With 24% of those indicating a mental health problem or illness.
- When asked “On a scale of 1 - 5, how affected are you by your caring role?” carers highlighted that they had felt extremely affected by tiredness, disturbed sleep, general feelings of stress, under physical strain, short tempered and had felt an existing condition worsen.
Figure 1: Graphic showing carers responses when asked "On a scale of one to 5, how affected are you by your caring role?"
- Carers told us that they often don’t have time to address their own health concerns and that they struggle to fit in health appointments for themselves due to a lack of time away from caring.
- In terms of describing their situation, 64% felt they were either neglecting themselves or sometimes are not able to look after themselves well enough.
- 47% of carers rated their overall quality of life as just being alright, with 21% stating this as being bad or very bad.
- Over 35% of people said that they have little social contact and feel socially isolated. “It’s a lonely tiring life and it wears us down massively”.
- Just over 70% stated that they felt able to spend time doing some of the things they value and enjoy but not enough and they enjoy some control over their daily lives but not enough.• 16% felt that they have no control over their daily life.
Experiencing loss
Former carers can find it hard to adjust to changes in their life when their caring role ends. Although caring often ends when the person being cared for dies, it may also be because the cared for person has moved into residential care, is being looked after by someone else or they no longer require looking after.
Whatever the circumstances this can leave a big gap in a carers life and can bring on very mixed emotions from relief at having some time to themselves, to guilt at feeling that way, to wanting to make some big changes, to feeling exhausted and alone and unable to cope and do much at all.
As well as coping with the loss of the person they have looked after, carers may find they also need to cope with the loss of their caring role and the changes they have to adjust to as they “rebuild” their life.
When a caring role ends this may also mean that the relationships carers have built up with professionals and friendships developed with peers also come to an end and they often feel isolated after many years of caring.
It is important to acknowledge the impact that loss, whatever the circumstance, has on a carer’s health and wellbeing and that they need continued support at this next stage of their carer journey.
What engagement with carers and stakeholders told us
- “Being a carer is life changing but being a bereaved carer can also be devastating especially when your sole purpose prior to this was to be there for your loved one”.
- One bereaved carer likened the loss to PTSD.
- “Making the decision to move mum into a care home was very difficult. The feelings of guilt were immense, I felt like I had let her down”.
- I cared for my wife around the clock - after she died, I was lost, I didn’t know what to do with myself and felt very alone”.
- “My whole identity changed over-night”.
- Carers also told us that they need continued support when their caring role has ended and this needs to be recognised.
The impact of Coronavirus on carers physical and mental health
Carers’ physical and mental health is often impacted by their caring role. The 2011 Census and the more recent GP patient survey by NHS England have shown that carers were more likely than non-carers to have poor health before the COVID-19 pandemic.
Nationally, the COVID-19 pandemic has seen 81% of carers take on increasing hours of care, often with less or no outside support . This has had a significant and detrimental impact on carers’ health and wellbeing; over two-thirds of carers (69%) reported that their mental health has worsened, and 64% of carers said their physical health has got worse as a result of caring during the pandemic.
What engagement with carers and stakeholders told us
Carers who responded to our local survey said that the pandemic had a negative impact on their own health and well-being:
- Over 70% stated that the pandemic had affected their mental wellbeing and led them to worry more about the person they are caring for, with over 30% feeling unsupported in their caring role.
- In relation to whether the pandemic had affected their own physical health, over 25% felt that this had affected them physically.
- 64% highlighted that they felt that COVID-19 had increased their caring responsibilities. “Isolating meant no external respite”.
- 33% stated that they felt the pandemic had affected their ability to be a carer which led to feelings of anxiety and guilt.
- Carers also told us that as the condition of the person they cared for got worse, their levels of exhaustion and anxiety rose and were impacting on their own health.
What we aim to do
- Work with the Mental Health Partnership Delivery Group to improve the offer of support to help carers address emotional and wellbeing needs, this should include carers who are also experiencing loss/bereavement.
- Review the practical support offered such as form filling, etc to help reduce the burden/stress on carers.
- Improve access to training and other preventative support and information to help carers stay healthy and care safely.
- Improve support options to enable carers to get to their own health appointments and access regular health checks ie short breaks, sitting services.
- Ensure the Carers Assessment asks carers how their caring role affects them and their health and wellbeing, so they can access the relevant support.
- We will look at how carers can be provided with affordable and flexible opportunities to take part in activities, which contribute towards good health and wellbeing. This will involve working with partners such as local leisure centres, colleges, the area councils and community groups/connectors.
- Make it easier for carers to access local services that could support their overall wellbeing and reduce their sense of isolation and loneliness
- Work closely with the primary care and the social prescribing service to support them to recognise the wider needs of carers and how these can impact on their physical and mental health to assist in signposting and referrals to support.
- We aim to improve the digital offer for carers as a mechanism for improving access to health and wellbeing information for those who are able/choose to use digital platforms.
Priority 5 – Carer's breaks
Carers are given the opportunity to discuss with practitioners and support staff the value of having a break from caring and the options available.
Caring for a family member, friend, or neighbour can be challenging and often comes at significant personal cost. Without sufficient support or meaningful breaks, it can take its toll on carer's emotional and physical health, their ability to work and have a knock-on effect on their long-term finances. A common theme arising from the consultations held with carers was not being able to have a break from their caring responsibilities.
What engagement with carers and stakeholders told us
- Carers need and value breaks away from their caring role. “I have no time for myself to do the things I enjoy.”
- Of those responding to the Carers' Survey, when asked what type of support would be most helpful to them as a carer, 37% said practical support such as short breaks or a sitting service and 29% said respite.
- Over 35% of people responding to the Carers' Survey said that they have little social contact and feel socially isolated.
- Many carers are reluctant to place their cared for person in residential care for their respite. Many give examples of negative experiences of this for the cared for person. “I will have to find another care home. He can’t go there again. I just need one break a year and then sitting service support so that I can carry on being on various committees in Barnsley, where I feel I make a difference and I enjoy this. If I didn’t have these to attend, I would be trapped at home. I don’t like the person I have become.”
- A survey carried out by the British Legion highlighted that less than one in ten carers in the armed forces community have been able to take a break from caring in the last year (9%), - this was even lower if the carer was caring for a veteran (4%).
- Carers have expressed that respite/short break opportunities are limited and difficult to access unless the person they care for is receiving support. The range of respite options appears to be quite limited.
- Information regarding how to access respite/short breaks and what is available needs to be clearer. It is difficult for carers to plan breaks not knowing if and what respite is available.
- Respite often comes too late when carers are already at crisis point - at this point the carer doesn’t get the same benefit from the break.
- Lack of respite opportunities is a constant theme of discussion at the Carer Forum meetings, where carers talk about “losing their identity” and “not having enough time for themselves”.
What we aim to do
- Work with commissioners in adult social care to look at the current offer around respite provision and direct payments for carers to enable them to access flexible short breaks and respite.
- Work with the disabled children’s team to look at the current offer around respite provision and direct payments for parent carers.
- Review the annual one-off payment grant for adult carers and how this can support short breaks.
- Work with the area councils and voluntary sector providers who deliver universal services/groups to ensure support in the community provides a variety of options for carers to have a break from caring and are less socially isolated.
Priority 6 – Helping carers stay in work
Carers are offered supportive working arrangements by workplaces.
The census 2011 identified that around one in nine working people are also carers and that the largest proportion of carers are in employment, whether full or part time. Yet we know that many carers experience substantial challenges in balancing employment and caring.
Without the right support, as many as one in six carers will have to give up work or reduce their working hours to care.
It is important that carers have support in the workplace so that they can manage the care they provide alongside their job. There are some simple steps that employers can take to reduce the feelings of isolation, stress and anxiety that carers experience and to ensure that they are able to balance work with their caring responsibilities.
What engagement with carers and stakeholders told us
- There is a lack of support from some employers including taking leave and an understanding of what a caring role entails.
- Some carers find it difficult to balance work and their caring role reporting that they are “stressed and exhausted”.
- Carers who are self-employed said they also need support besides those who're in paid work.
- More out of hours support to accommodate working carers is needed. “Barnsley Carers Service provide home visits and early morning support to work around my work hours.”
- Support for carers should be included in occupational services and employee assistance programmes so employees who are carers can access support through work.
- In terms of employment status, 30% of people who responded to our Carers' Survey work in paid roles and said that they felt supported as a carer by their employer. 12% did not feel supported by their employer. “I have had to change jobs five times in the last five years so that I can support my mum and dad in their home. Dad died last year, and mum needs more help than ever. I feel like I am running two homes. I make all of the household decisions for my mum and have my own family and work to juggle.”
- 28% of people stated they are not in paid work due to their caring responsibilities.
What we aim to do
- Work with health partners and employers across the borough to raise awareness of carers issues and promote flexibility in the workplace for employees with caring responsibilities.
- Building on the carer action plan developed by Barnsley Council’s human resource team we will support employers across the borough by;
- Developing carer's guidance and/or toolkits which include a clear definition of what a carer is.
- Providing advice and information on the law.
- Support to implement carer friendly policies and flexible working practices in the workplace including time off to attend appointments with the cared for person.
- Helping managers to identify carers within their teams and help staff identify themselves as carers.
- Providing links to sources of information and advice for employees, such as that provided by Carers UK as well as local information, ensuring that they are accessible to employees.
- Work with employers across the borough to consider the implementation of employment carer passports.
Priority 7 – Young carers
Support young carers from inappropriate caring and provide the support they need to help them balance their caring role with their rights to be children or young people.
It is important that we recognise young carers and young adult carers as children and young people in their own right and minimise the potential negative impact of caring responsibilities on their life chances.
Many young people within Barnsley are helping to care and the person being cared for will usually be a family member such as a parent, grandparent, sibling, or someone very close to the family. The person or people they care for will have a serious or long-term illness, disability, mental health difficulties or problematic use of alcohol or drugs; many young carers also help to care for younger siblings.
Our young carer's needs will be included in all the key priority areas of this strategy as there will be generic support needs, challenges and areas for change that will be just as relevant to a young carer as an adult carer. However, we acknowledge that there are also some differences in how we identify young carers and the types of support they require. Therefore, this section will focus on the specific outcomes that we want to achieve for young carers.
The transition from young carer to young adult carer at the age of 18 years needs to be carefully managed. Young adult carers need to continue to be supported in their role, whilst also encouraging them to take their next steps into employment or continued education and training. Robust transitional arrangements will be a priority for children and adult social care, the Young Carers Service, and the newly commissioned Adult Carer Support Service.
What engagement with young carers and stakeholders told us
- They want access to good quality information and advice, and to not be disadvantaged by the role of the carer.
- They want a better understanding of more of the services and policies that support people in their role as a carer and have the ability to influence and contribute to these.
- They want to be fully supported during transitions to key services and understand the differing arrangements and options for support and breaks.
- They want to ensure education and training is available to support all members of our communities to raise awareness and value the role of carers.
- They want support to continue to lead and enjoy their own life through work and play.
- They feel that the recognition of carers and their contribution to health and wellbeing of those they care for needs to be improved.
- They need to remain safe within their role and free from harassment in the wider community.
- They would like to participate fully in their community and increase social connections.
- They feel it is important that they have the knowledge and skills necessary to support those they care for.
- They value the support received from the Young Carers Service:
- “YC is really, really good it gives you advice and support. It’s tailored to support you.”
- “I am much better at dealing with my worries and concerns, the tools I have been given are great. Thank you will never be enough.”
- “Young Carers is a really good group. They make you feel very welcome. They are really understanding and help you understand things that are really hard to talk about.”
What we aim to do
- Raise the profile of young carers at a strategic and operational level.
- Develop and implement processes for early identification, referral, assessment and support.
- Enable young carers to co-produce and co-deliver solutions in the improvement and delivery of services.
- Work with health care providers to ensure that young carers are valued and seen as part of health care processes.
- Ensure young carers are supported in education and during key transition points ensuring robust transitional arrangements are in place.
- Develop universal provision and positive opportunities to support young carers outside of their caring roles and be treated as individuals in their own right.
- Promote the health and wellbeing of young carers including emotional and physical wellbeing.
Priority 8 – Parent carers
Work is currently taking place with the Barnsley SEND Parent and Carers Alliance to co-produce this priority.

