Health improvement and inequality continue to be a challenge for the borough and this is influenced by a number of factors outside the direct influence of health care.
The things that make us healthy include good work, education, resources, our physical environment and social connections.
As little as 10% of the population's health and well-being is linked to access to health care. We need to look at the bigger picture:
- good work
- our surroundings
- money and resources
- housing
- education and skills
- the food we eat
- transport
- family, friends and communities
Health care
This section includes:
- cardiovascular disease (CVD)
- cancer
- liver disease
- NHS health checks
- respiratory conditions
- sensory impairment - sight loss
Cardiovascular disease (CVD)
Why this is important
In the UK, cardiovascular disease causes a quarter of all deaths and is the largest cause of premature mortality in deprived areas. Those in the most deprived 10% of the population are almost twice as likely to die as a result of CVD, than those in the least deprived 10% of the population.
Falling mortality rates from heart disease were the main contributor to increases in life expectancy between 2001 and 2016 in England, according to the Health Profile for England. However, since 2011 the rate of increase in life expectancy has slowed for both males and females as improvements in heart disease mortality have plateaued. This highlights the need for a renewed drive to prevent CVD deaths, which still account for 1 in 4 of all deaths in England. (Health Matters: preventing cardiovascular disease, 2019)
In Barnsley, CVD is a major contributor to health inequalities. The age sex standardised mortality for CVD in those aged under 75 is 20% higher than the national average (2016-2018).
In January 2017, the commissioning for Value (CfV) ‘Where to Look Pack’ stated that CVD is the biggest opportunity for the Barnsley health economy when health outcomes and spend are combined. It highlighted high non-elective admissions and associated spend for Cardiovascular Disease.
The Barnsley picture and how we compare
Risk factors
Sourced from: other JSNA profiles, PHE CVD Profiles
- Around 1 in 5 adults in Barnsley are smokers (18.3%), according to the national annual population survey (2019). This is significantly higher than the England rate of 13.9%.
- Almost three-quarters (73%) of Barnsley adults are overweight or obese, significantly higher than the national average (62.8%).
- Latest data (2019/20) indicates that more than a quarter (28.7%) of Barnsley adults are physically inactive (doing less than 30 minutes physical activity per week). This is significantly higher than the national rate of 22.9%.
- More than a quarter (28.4%) of adults (18+) in Barnsley report drinking over the recommended 14 units of alcohol each week, similar to the England rate of 22.8%.
- In 2019/20, 15.6% of Barnsley’s GP registered population were recorded on practice registers with hypertension (high blood pressure), significantly higher than the England rate of 1%.
Diabetes
Sourced from: PHE CVD Profiles
- In 2019/20, 7.7% of Barnsley’s GP registered population aged 17+ (16,496 people) were recorded on practice registers with diabetes, significantly higher than the England rate of 1%.
- Compared to 10 similar Clinical Commissioning Groups (CCGs), Barnsley’s rate is the third lowest.
- Rates have increased at each time point since 2009/10.
- Barnsley’s estimated prevalence of diabetes (diagnosed and undiagnosed) is 8.8% of the practice population (18,512 people). This means that there are an estimated 2,016 people registered on Barnsley GP registers expected to have diabetes, who have not been diagnosed.
- Of the people in Barnsley who are registered with Type 2 Diabetes, just over half (56.8%) are male; this reflects the overall England proportion (55.9% male).
Stroke
Sourced from: PHE CVD Profiles, Local Health
Prevalence
- In 2019/20, 2.2% of Barnsley’s GP registered population (5,823 people) were recorded on practice registers with stroke or transient ischaemic attack (TIA), significantly higher than the England rate of 8%.
- Compared to 10 similar Clinical Commissioning Groups (CCGs), Barnsley’s rate is the third highest.
- Rates have remained fairly constant since 2009/10.
Hospital admissions
- Barnsley’s 2019/20 hospital admissions rate for stroke (276.0 per 100,000) is significantly higher than the England rate of 170.2 per 100,000 and the highest when compared to similar CCGs.
- The current rate equates to 675 hospital admissions in 2019/20 for Barnsley residents for stroke.
- At ward level, the rates in North East, Darfield, St Helens, Worsbrough and Monk Bretton wards were more than one and a half times higher than the England rate.
Mortality
- Although Barnsley’s rates for under 75 mortality from stroke have fallen over recent years, the 2017/19 rate of 15.7 per 100,000 is still significantly higher than the England rate of 12.5 per 100,000.
- Compared to 10 similar Clinical Commissioning Groups (CCGs), Barnsley’s rate is the fifth highest.
- At local level, Worsbrough and North East wards have significantly higher mortality rates from stroke than the England average.
Heart
Coronary heart disease (CHD)
Prevalence
- In 2019/20, 4.3% of Barnsley’s GP registered population (11,467 people) were recorded on practice registers with CHD; significantly higher than the England rate of 3.1%.
- Compared to 10 similar Clinical Commissioning Groups (CCGs), Barnsley’s rate is the second highest.
- Rates have shown a consistent downward trend since 2009/10.
Hospital admissions
- Barnsley’s 2019/20 hospital admissions rate for CHD (695.1 per 100,000) is significantly higher than the England rate of 469.9 per 100,000 and the second highest when compared to similar CCGs.
- The current rate equates to 1,740 hospital admissions in 2019/20 for Barnsley residents for CHD.
- At local level, all wards had significantly higher admission rates in 2015/16-2019/20 than the England average, with the rates in Dearne South, Wombwell, Kingstone, Stairfoot, Royston, Dearne North, Worsbrough, St Helens and Cudworth being more than twice as high as England.
Mortality
- Although Barnsley’s rates for under 75 mortality from CHD have fallen over recent years, the 2017/19 rate of 47.5 per 100,000 is still significantly higher than the England rate of 37.5 per 100,000.
- Compared to 10 similar Clinical Commissioning Groups (CCGs), Barnsley’s rate is the fifth highest.
- The rate has reduced by more than half since 2003/05.
- At local level, Penistone East has a significantly lower rate than the England rate. The highest rate is in St Helens.
Heart failure
Prevalence
- In 2019/20, 1.1% of Barnsley’s GP registered population (3,033 people) were recorded on practice registers with heart failure; slightly higher than the England rate of 9%.
- Rates have shown a consistent upward trend since 2009/10.
Hospital admissions
- Barnsley’s 2019/20 hospital admissions rate for heart failure (212.3 per 100,000) is significantly higher than the England rate of 171.8 per 100,000 and the third highest when compared to similar CCGs.
- The current rate equates to 510 hospital admissions in 2019/20 for Barnsley residents for heart failure.
Kidney
Prevalence
- In 2019/20, 4.1% of Barnsley’s GP registered population (8,626 people) were recorded on practice registers with Chronic Kidney Disease (CKD); similar to the England rate of 4.0%.
- Compared to 10 similar CCGs, Barnsley is ranked 4th
- Rates have shown a consistent downward trend since 2010/11.
Renal Replacement Therapy (RRT)
- In 2018, 256 of Barnsley’s GP registered population were receiving RRT, an increase of 21% since 2012.
- Of the 256 people receiving dialysis, 51.2% had a kidney transplant, 9.0% were receiving home dialysis and 39.8% were receiving hospital dialysis.
Mortality from all CVD
Sourced from PHOF E04a and Local Health
Under 75 mortality from all CVD
- Although Barnsley’s rates for under 75 mortality from CVD have fallen over recent years, the 2017/19 rate of 89.3 per 100,000 is still significantly higher than the England rate of 70.4 per 100,000.
- Compared to similar local authorities, Barnsley is ranked 6th out of 16 (where 1 is the highest).
- The rate has reduced by half since 2001/03.
- At local level, there are large geographical differences. Compared to the England average, the under 75 mortality rate in St Helens ward is more than twice as high, whilst the rates in Darton West is significantly lower.
Under 75 mortality from CVD considered preventable
Sourced from PHOF E04b
- In terms of under 75 mortality from CVD that is considered preventable, Barnsley’s 2017/19 rate of 34.6 per 100,000 is significantly higher than the England rate of 28.2 per 100,000.
- Compared to similar local authorities, Barnsley is ranked 10th out of 16 (where 1 is the highest).
- The rate has reduced from 81.3 per 100,000 in 2001/03.
Contribution of CVD mortality (all ages) to the gap in life expectancy between Barnsley and England
Sourced from PHE Segment Tool
- When considering the life expectancy gap between Barnsley and England in 2015/17, CVD accounted for 22.7% of the gap for men and 20.5% for women. In terms of numbers, this means that during 2015/17, there were 153 more deaths from CVD (95 males, 58 females) than if Barnsley had experienced the same mortality rate as England.
Contribution of CVD mortality (all ages) to the gap in life expectancy between the most deprived quintile and the least deprived quintile of Barnsley
Sourced from PHE Segment Tool
- When considering the life expectancy gap between the most deprived quintile and the least deprived quintile of Barnsley in 2015/17, CVD accounted for 30.8% of the gap for men and 19.3% for women. In terms of numbers, this means that during 2015/17, there were 190 more deaths from CVD (118 males, 72 females) in the most deprived quintile of Barnsley than if it had experienced the same mortality rates as the least deprived quintile.
Data from:
What we're doing and the assets or services we have
A local Cardiovascular Disease Health Needs Assessment was completed in 2021 which focussed on risk factors for CVD and the identification and management of heart diseases. The key recommendations from this report were used in the development of a new Heart Health Action Plan for Barnsley. It was decided that the term heart health be used instead to CVD in order to make it more accessible and understandable to all.
Subsequently, a new Heart Health Alliance group was established in September 2021 to embed new ways of partnership working and to oversee delivery of the new Heart Health Action Plan. Partners represented included; BHNFT, SWYPFT, BMBC, BCCG. The vison of the group is to prevent, detect early and successfully manage heart health diseases to enable the people of Barnsley to live as long as possible in good health.
Key principles for the Heart Health Alliance are to identify any opportunities to shift more towards primary prevention (ie prevention of disease in the first place through healthy lifestyle factors) and to consider addressing any inequalities in outcomes in every action.
We understand heart health is strongly associated with health inequalities. People living in the most deprived areas are almost 4 times more likely to die prematurely than those living in the least deprived. To tackle this, Public Health has undertaken a population approach to empower communities within Barnsley to be able to make the healthy choice the easy choice which will lower the risk of CVD. An example of which being we have worked with Barnsley Hospital to successfully implement the QUIT programme, making it a smokefree site. Targeted work with the hardest to reach communities will be undertaken to reduce heart health risk factors and to encourage early identification of heart health issues.
Barnsley CCG’s Health Improvement Nurse supports practices with targeted support in order to decrease variation between practices and communities and support the detection and management of high risk heart health conditions such as atrial fibrillation, high blood pressure and raised cholesterol. This includes the development of practice profiles for each practice including peer comparison data.
Opportunities for improvement or future development
Ongoing delivery of the new Health Heart Action Plan through the Heart Health Alliance partnership group. Identification of the very latest data available to assess the current picture of Heart Health in Barnsley post Covid-19 and to create a framework in order to monitor progress in heart health prevention.
Resources and supporting documents
Cancer
Why this is important
Cancer accounts for more than a quarter (26.4%) of all deaths for the people in Barnsley and continues to affect many people in Barnsley who are living with the after effects of having a cancer diagnosis.
Lung cancer is responsible for the greatest proportion of cancer deaths in Barnsley (24.2% of all male and 24.4% of all female cancer deaths). 72% of lung cancer cases in the UK are caused by tobacco use; the largest contributor to preventable deaths. For men in Barnsley, prostate cancer is the second largest cause of death, being responsible for 11.8% of all male cancer deaths. In women, breast cancer is the second major cause of death from cancer, accounting for 12.4% of all female cancer deaths. Head and Neck cancers are also high rates for Barnsley
An ageing population and a rise in lifestyle risk factors mean that the number of people being treated with cancer is expected to rise. Nearly 4 in 10 cancer cases in 2015 were attributable to known risk factors - smoking, alcohol and physical exercise. Screening rates have improved across Barnsley, however, this is not translating into the improved outcomes that we would expect to see in terms of cancers diagnosed at early stage and 1- and 5-year survival rates. More work is required to ensure that those who are most at risk are supported to understand that risk and to participate in the programmes. It is also important that people know the early signs of cancer and go to their GP Practice if they suspect cancer.
The Barnsley picture and how we compare
Risk factors
- Around 1 in 5 adults in Barnsley are smokers (18.3%), according to the national annual population survey (2019). This is significantly higher than the England rate of 13.9%.
- The proportion of dependent drinkers in Barnsley (1.89%) is significantly higher than the national rate of 1.39%.
- Barnsley’s 2020/21 rate for hospital admissions for alcohol-related conditions (546 per 100,000 population) is significantly higher than the England rate of 456 per 100,000.
- Latest data (2019/20) indicates that almost three-quarters (73%) of Barnsley adults are overweight or obese, significantly higher than the national average (62.8%).
Incidence (new cancer cases)
- In 2019/20, Barnsley’s cancer incidence rate was 578 new cases per 100,000 population; higher than the England rate of 531 per 100,000. In terms of numbers, this equates to 1,521 people on Barnsley GP registers who were diagnosed with cancer in 2019/20.
- Compared to 10 similar Clinical Commissioning Groups (CCGs), Barnsley’s rate was the sixth lowest.
- In terms of incidence by tumour type, Barnsley has a significantly higher rate than the England average for lung cancer and a significantly lower rate for prostate
- Large geographical differences exist within Barnsley, with incidence rates (for all cancers) in Darfield ward being significantly higher than the England average and the incidence rate in Penistone East ward being significantly lower.
- For breast cancer, the incidence rate in Dearne South ward in 2014-2018 was almost one and a half times higher than the England rate.
- For colorectal cancer, the incidence rate in Darfield ward in 2014-2018 was almost one and a half times higher than the England rate.
- For lung cancer, the incidence rate in St Helens ward in 2014-2018 was more than double the England rate. Eight more wards (Cudworth, Stairfoot, North East, Wombwell, Royston, Worsbrough, Darfield and Central) had significantly higher rates than the England average. Only Dodworth, Penistone East and Penistone West wards had lower incidence rates than the England average.
- For prostate cancer, all wards had lower incidence rates than the England average in 2014-2018, with the rates in North East, Dearne North, Royston, Monk Bretton, Wombwell, Hoyland Milton, Rockingham, Kingstone and Central being significantly lower.
Prevalence (people with cancer, as recorded on practice disease registers)
- In 2019/20, 3.2% of Barnsley’s GP registered population were recorded as having a diagnosis of cancer, similar to the England rate of 3.1%. In terms of numbers, this represents 8,378 people on Barnsley GP registers who have had a diagnosis of cancer.
- Compared to 10 similar CCGs, Barnsley’s rate is the joint second lowest.
- Rates have increased over recent years (from 2.1% in 2012/13).
Screening
- Barnsley’s 2021 breast screening rate (females, 53-70) of 55.4% is significantly lower than the England rate of 64.1%.
- Out of 16 similar local authorities, Barnsley’s rate is the third lowest.
- The current rate is the lowest since 2010.
- At GP practice level, screening rates range from 7.0% to 78.1%.
- Barnsley’s 2021 cervical screening rate (females, 25-49) of 75.1% is significantly higher than the England rate of 65.2%.
- Out of 16 similar local authorities, Barnsley’s rate is the
- At GP practice level, screening rates range from 63.0% to 84.2%.
- Barnsley’s 2021 bowel screening rate (persons, 60-74) of 67.4% is significantly higher than the England rate of 63.8%.
- Out of 16 similar local authorities, Barnsley’s rate is the
- The 2021 rate of 67.4% is the highest since 2015.
- At GP practice level, screening rates range from 58.9% to 78.0%.
Two week wait referrals
- Barnsley’s 2020/21 rate for two week wait referrals for suspected cancer (3,526 per 100,000 population) is higher than the England rate of 3,389 per 100,000. In terms of numbers, this equates to 9,318 urgent referrals for suspected cancer made for patients registered at Barnsley GP registers in 2020/21.
- Compared to 10 similar CCGs, Barnsley’s rate is the fifth highest.
- At GP practice level, two week wait referral rates per 100,000 range from 940 to 5,957.
- Less than half (44.7%) of patients in Barnsley treated for cancer in 2016/17 – 2020/21, were referred through the two week wait referral route; a significantly lower proportion than the England rate of 52.9%.
- At GP practice level, proportions of patients treated for cancer who were referred through the two week wait referral route range from 20.0% to 75.0%.
Emergency presentation
- Latest data (2020/21 Q4) shows that 24.8% of all malignant cancer diagnoses in Barnsley were diagnosed as an emergency, compared to 21.0% in England overall.
- Barnsley’s rates have fluctuated since 2016, but have been higher than the England average at each time point.
Staging
- Latest staging data (2019) shows the percentage of cancers diagnosed at stage 1 or 2 was 50.1%, significantly lower than the national average of 55.1%.
- If a person is diagnosed at stage 2 for lung cancer, 60% will survive their cancer for a year or more after diagnosis whereas for stage 4 it is only 20%.
- For stomach cancer, more than 40% will survive their cancer for 5 years or more compared to being diagnosed at stage 4, which is 5%.
Survival
All cancers
- More than 7 out of 10 (72.1%) adults (aged 15-99 years) in Barnsley who were diagnosed with cancer (all cancers) in 2017 were still alive one year after diagnosis. However, Barnsley’s 1-year survival rate is significantly lower than the England rate of 73.3%.
- 1-year survival rates within similar CCGs range from 70.0% to 74.0%.
- Barnsley’s rates have improved over recent years (from 59.5% in 2002).
- 1-year survival rates are higher in the younger age groups:
| Area | 15-44 years % | 45-54 years % | 55-64 years % | 65-74 years % | 75-99 years % |
| Barnsley | 88.3 | 83.4 | 78.3 | 70.9 | 59.9 |
| England | 89 | 84.2 | 79.3 | 72.7 | 60.8 |
Breast cancer
- Of the adults (aged 15-99 years) in Barnsley diagnosed with breast cancer in 2017, 97.5% were still alive one year after diagnosis; slightly higher than the England rate of 97.0%.
- Compared to 10 similar CCGs, Barnsley’s 1-year survival rate for breast cancer is the second highest.
Bowel cancer
- Four out of five (80.4%) adults (aged 15-99 years) in Barnsley diagnosed with bowel cancer in 2017 were still alive one year after diagnosis; slightly lower than the England rate of 80.7%.
- 1-year survival rates for bowel cancer within similar CCGs range from 75.6% to 83.9%; Barnsley’s rate is the fourth highest.
Lung cancer
- Less than half (42.5%) of adults (aged 15-99 years) in Barnsley diagnosed with lung cancer in 2017 were still alive one year after diagnosis; slightly lower than the England rate of 43.1%.
- 1-year survival rates for lung cancer within similar CCGs range from 39.6% to 44.7%.
Patient experience
- On a scale of 0 (very poor) to 10 (very good), the average rating for Barnsley CCG cancer patients for their overall experience of care in 2018 was 8.9.
Mortality
- During 2019-2021 in Barnsley, 2,129 people were registered as dying from cancer, accounting for more than a quarter of all deaths.
- Lung cancer is responsible for the greatest proportion of cancer deaths in Barnsley (24.2% of all male and 23.0% of all female cancer deaths).
- In men, prostate cancer is the second largest cause of death from cancer, being responsible for 11.1% of all male cancer deaths.
- In women, breast cancer is the second major cause of death from cancer, accounting for 13.0% of all female cancer deaths.
Under 75 mortality from cancer
- Although Barnsley’s rates for under 75 mortality from cancer have fallen over recent years, the 2017/19 rate of 142.0 per 100,000 is still significantly higher than the England rate of 129.2 per 100,000.
- At ward level, there are large geographical differences, with rates per 100,000 (2015/19) ranging from 100.3 in Penistone East to 184.9 in Dearne North. The rates in Darton West and Penistone East wards are significantly lower than the Barnsley average.
Under 75 mortality from cancer considered preventable
- In terms of under 75 mortality from cancer that is considered preventable, Barnsley’s 2020 rate of 58.7 per 100,000 is similar to the England rate of 51.5 per 100,000.
Data from:
- PHE Cancer Services profile
- Public Health Outcomes Framework
- PHE Local Health
- PHE National General Practice Profiles
- ONS Index of cancer survival
- National Cancer Registration and Analysis Service: Cancer Outcome Metrics
- National Cancer Patient Experience Survey 2018 - National and Local data
What we’re doing and the assets and services we have
The Barnsley Cancer Programme aims to improve the whole cancer pathway, from raising awareness, to support at end of life via an integrated approach. The Programme is delivered in partnership between the South Yorkshire Cancer Alliance, NHS Barnsley CCG, Barnsley Hospital NHS Foundation Trust (BHNFT), South West Yorkshire Partnership NHS Foundation Trust (SWPFT), Barnsley Council, Cancer Research UK, Macmillan, NHS England and Voluntary Sector groups and the public of Barnsley.
The Barnsley Cancer Programme oversees five key work streams which are listed below with example projects.
Prevention
A key work is supporting the prevention of cancer by raising with primary care and community staff the early signs of cancer; encouraging people to present early, increasing the number of people to attend for screening via a variety of services; and promoting communities to have a healthy lifestyle. There are also several projects running that are emphasising to people the importance of having regular exercise, reducing alcohol intake and how having a healthy diet prevents cancer.
Early diagnosis
To support early diagnosis and better outcomes for people living with cancer, I-Heart Barnsley runs a clinic at the weekend for cervical screening sessions. The service is for local people to fit their cervical screening appointments around their busy schedules. There will also be breast screening services running at the town centre Glassworks Community Diagnostic hub and increased clinic slots due to having an additional machine being available. This will make it more accessible for people to attend for appointments. In 2022 the programme is also running a behavioural insight nudge work, to nudge people who have not come forward during the pandemic to present at their GP practices and also if they have been referred to not delay their attendance at hospital. Navigators and Co-ordinators have been introduced to provide patient with 1-2 people who will be a point of contact for the person. Work is also taking place to ensure people who have suspected cancer referrals have a diagnosis within 28 days and the introduction of a cancer exclusion test (FIT) in primary care has been implemented.
Best treatment and care
Linking to best treatment and care, a teledermatology service has been commissioned to identify skin cancer early. BHNFT continue to employ cancer support workers to provide patients to have personalised care when they are diagnosed and going though treatment. An additional chemotherapy location has opened in the town centre in addition to Weston Park in Sheffield and at the hospital; the introduction of less invasive treatments that may have a long-term health impact on the person and increasing activities at the “Well Centre” for people who are going through treatment.
Personalised care
This work includes the recovery package, remote monitoring, health and wellbeing care, stratified follow up pathways and timely re-access to cancer support. Cancer Support Workers are in place (to support the patients’ journey and to complete regular holistic needs assessments), as well as an anxiety management training programme for Barnsley patients. This includes a programme of work looking at enabling patients to ‘live well’ after a cancer diagnosis – right up to curative or end of life care, specifically in Colorectal, Lung; Urology and Breast cancer.
End of life
To support best care at end of life, the Hospice has introduced a self-management 6 week programme for people considered at end of life within the next 9-12 months. Patients continue to inform services that having early advanced care planning at EOL makes a difference to their quality of life and choosing where they wish to die. Services have been working on supporting people to make these choices by using the Electronic Palliative Care Co-ordination System (EPaCCS) throughout primary care and community care in Barnsley. EPaCCS is a communication tool that enables palliative patients and those closest to them to have their preferences and wishes for their care and subsequent place of death discussed and recorded, to have clear treatment and escalation plans that will guide health and social care providers to deliver the right care, in the right place by the right people. The Advanced Nurse Practitioner continues to work with people living in care homes to increase their choice about end of life wishes. This has led to a reduction in avoidable admissions to hospital and an increase in dying in their place of choice.
Opportunities for improvement or future development
The Barnsley Cancer Programme continues to develop initiatives to improve the cancer pathway for Barnsley people. Future developments include increasing easier access to diagnostic tests within the community via the Glassworks Community Diagnostic hub – this provision will enable people to receive diagnostic tests for cancer from a town centre location rather than a hospital and the on-stop straight to test timed pathways which aim for potential cancers to be diagnosed more quickly.
Resources and supporting documentation
Liver disease
Why this is important
The liver is our largest internal organ and it has hundreds of different roles, including the breakdown of food into energy and helping the body get rid of waste products and fight infections - particularly in the bowel. And yet, when your liver is damaged, there are generally no symptoms- until things get serious*
Liver disease is one of the top causes of death in England and people are dying from it at younger ages. Liver disease is largely preventable. Whilst approximately 5% is attributable to autoimmune disorders (diseases characterised by abnormal functioning of the immune system), most liver disease is due to three main risk factors: alcohol, obesity and viral hepatitis. Overall, alcohol-related liver disease accounts for well over a third (37%) of liver disease deaths. And figures show victims of liver disease are getting younger. More than one in 10 of deaths of people in their 40s are from liver disease, most of them from alcohol-related liver disease**.
In Barnsley, liver disease mortality rates have increased consistently throughout recent years and now for the first time across 18 years of comparative data, we have significantly higher rates than the England average.
References
* British Liver Trust website. About The Liver. The Information Standard member organisation.
** National End of Life Care Intelligence Network website. Deaths from Liver Disease: Implications for end of life care in England.
The Barnsley picture and how we compare
Hospital admissions
- In 2019/20, the hospital admission rate due to liver disease in Barnsley was 148.7 per 100,000. This is similar to the England rate of 143.6 per 100,000.
- Barnsley has the 7th highest rate for hospital admissions due to liver disease across the 15 areas of Yorkshire and the Humber.
- In terms of numbers, the rate of 148.7 represents 365 admissions to hospital of Barnsley residents due to liver disease in 2019/20. There were more than twice as many admissions for men than women (250 compared to 115).
- The 2019/20 rate of 148.7 is the highest since 2010/11.
Mortality
(PHOF E06a and Mortality Profile – by gender)
- Barnsley’s 2017/19 under 75 mortality rate from liver disease (21.7 per 100,000) is similar to the England rate (18.5 per 100,000).
- Barnsley has the sixth highest rate for liver disease mortality across the 15 areas of Yorkshire and the Humber.
- The rate for men (29.0 per 100,000) is double that of women (14.5 per 100,000).
- Rates have increased over recent years (from 12.9 per 100,000 in 2001/03).
- At ward level (2015/19), under 75 mortality rates from liver disease per 100,000 range from 5.5 in Penistone East to 37.3 in Monk Bretton ward.
Alcohol-related liver disease
- Across the Yorkshire and Humber region Barnsley has the fourth highest rate of under 75 mortality from alcohol-related liver disease.
- Despite having a higher mortality rate for under 75 alcoholic liver disease than the regional and national averages, the rate of hospital admissions for alcoholic liver disease in Barnsley are lower. This suggests that those people suffering with liver disease and ultimately dying in consequence are not being referred or admitted to hospital.
Resources
- Public Health England (Liver Disease Profiles)
- Public Health Outcomes Framework (E06a)
- Public Health Outcomes Framework (Mortality Profile)
- NHS Digital – Quality Outcome Framework - the prevalence of liver disease in the borough can be viewed through the Quality Outcomes Framework tool on the NHS Digital site. It also allows you to see data down to GP Practice level for a number of conditions.
- Public Health England - Premature mortality visualisation tool - the Longer Lives mortality tool highlights premature mortality across every local authority in England, giving people important information to help them improve their community's health. It includes data for liver disease.
What we're doing and the assets or services we have
We have identified liver disease as a key issue affecting the health and wellbeing of our residents. We are currently working towards thoroughly understanding the ‘who, when, where and how’. Following this, we will best placed to act with effective action. We are currently working towards:
- Prioritising a whole systems approach to reducing alcohol consumption and obesity as the key causes of preventable liver disease and early death.
- Improving awareness, prevention, early detection and treatment of liver disease.
- Further exploring liver-disease mortality and hospital admission rates.
- Reviewing case studies to help us develop appropriate plans.
Resources and supporting documents
- Liver Disease Profile (Christus Ferneyhough)
- National Institute of Health and Social Care Excellence (NICE) guidance - Liver conditions - NICE has produced a number of documents that cover liver disease including guidance on chronic liver disease, alcohol-use disorders, cirrhosis, liver cancer and non-alcoholic fatty liver disease.
- Public Health England (NICE) - Liver disease: applying All Our Health - evidence and information to help healthcare professionals raise awareness of risk factors for liver disease.
NHS health checks
Why this is important
In the UK, high blood pressure, smoking, cholesterol, obesity, poor diet, physical inactivity and alcohol consumption are the top seven causes of preventable death. The Department of Health estimates that the NHS health check programme prevents 1,600 heart attacks and 4,000 people from developing diabetes each year. It also detects 20,000 cases of diabetes or kidney disease earlier each year. Estimates suggest that the programme will pay for itself after 20 years and deliver substantial health benefits.
NHS health checks is a national programme commissioned by councils. Health checks offer people aged 40 to 74 a free check-up of their overall health, every 5 years. The results can tell people whether they are at higher risk of developing certain health problems, such as heart disease, diabetes, stroke and dementia. They help underpin the NHS long-term plan commitments to prevent 150,000 heart attacks, strokes and cases of dementia, and to increase take up of the NHS diabetes prevention programme.
During the check-up the individual’s risk of the above diseases will be assessed; support and advice or treatment will then be offered where necessary about reducing or managing risk. This approach provides a key route into existing lifestyle interventions through well-established pathways to support people to stop smoking, lose weight, be more active and drink within recommended limits as appropriate.
The Barnsley picture and how we compare
-
In 2018/19, almost half (48.1%) of people in Barnsley who were invited for an NHS Health Check took one up; significantly higher than the England rate of 45.9%.
-
Compared to similar authorities, Barnsley is ranked 8th out of 16.
- The rate of 48.1% equates to 3,693 people in Barnsley who had a Health Check in 2018/19, of which :
- 14.7% were current smokers
- 26.3% had a CVD risk higher than 10%
- 24.0% had high blood pressure
- 71.2% were an excess weight
- 24.3% had a high cholesterol ratio
- 69.3% were classified as active
- 37.0% were advised to reduce their alcohol intake -
The more deprived areas had a higher proportion of current smokers and a lower proportion of people classified as active (undertaking more than two and a half hours of physical activity a week).
Data from:
What we're doing and the assets or services we have
The provision of NHS health checks is a mandatory requirement for local authorities.
From April 2018 a new provider, Hallcross Medical was commissioned to provide NHS health checks in Barnsley. This resulted in a new service model approach in which the service is provided through a contract with a single provider.
Although GP invitations and involvement remain a key aspect of the health check provision, the new model now offers service outreach in community and business settings. The provider arranges opportunistic checks on eligible patients through workplaces and community events which allows for a more targeted uptake of health checks eg in deprived areas, with men, in routine and manual workforces etc. More recently, our provider has also been able to offer health checks via local pharmacies.
The delivery model specification for this service includes performance monitoring metrics. We hold quarterly contract and performance meetings with our provider where we receive progress reports and discuss their performance and any areas for improvement. We also feedback regionally to Public Health England on a quarterly basis.
Opportunities for improvement or future development
Nationally, the NHS Health Check programme has made progress during the last 10 years. However uptake varies across the country (NHS health check data), the risks identified in a check could be followed up more consistently and evidence is emerging that people could benefit from a more tailored service (for example: Lindbohm, J.V. et al (2019) 5-year versus risk-category-specific screening intervals for cardiovascular disease prevention: a cohort study).
There may also be a case for a particular focus on supporting people through key changes in their life, in particular thinking about future care needs and how they can remain healthy and active in older age.
The government’s green paper ‘advancing our health: prevention in the 2020s’ offers the next opportunity to further shift of focus from cure to prevention. As part of this there will be an opportunity to consider whether changes to the NHS health checks programme could help it deliver even greater benefits. The government will commission an evidence-based review of the programme to maximise the benefits it delivers in the next decade.
Resources and supporting documents
- NHS Health Check programme - a collaborative resource which brings together national and local resources aimed to support those involved in commissioning and providing NHS health checks.
- NHS health checks: Analysis of health checks delivered to Barnsley residents in 2018/19
Respiratory conditions
Why this is important
Respiratory conditions are one of the main contributors to reduced life expectancy in both males and females compared to England. Respiratory disease encompasses a range of conditions affecting the airways and structures of the lung. The most common serious acute respiratory disease is pneumonia, whilst chronic respiratory conditions such as asthma, chronic obstructive pulmonary disease (COPD), and respiratory allergies affect many people and are a major disease burden. It affects one in five people and is the third biggest cause of death in England (after cancer and cardiovascular disease). Lung cancer, pneumonia and chronic obstructive pulmonary disease (COPD) are the biggest causes of death.
Incidence and mortality rates from respiratory disease are higher in disadvantaged groups and areas of social deprivation, with the gap widening and leading to worse health outcomes. The most deprived communities have a higher incidence of smoking rates, exposure to higher levels of air pollution, poor housing conditions and exposure to occupational hazards.
As a former coal mining town in South Yorkshire (the last pit closed in 1991) a small proportion of the population may have or be at risk of developing pneumoconiosis (lung disease caused by dust). This disease takes a number of years to manifest and usually develops 10-20 years after exposure, although the timescales can be less if the individual is subject to heavy exposure.
Chronic obstructive pulmonary disease (COPD) is the name for a collection of lung conditions including chronic bronchitis and emphysema. COPD leads to damaged airways in the lungs. This causes the airways to become narrower, making it difficult for air to move in and out of the lungs. COPD is treatable, but not curable. Identifying and treating COPD early can slow down the decline in lung function, and so lengthen the period of time in which someone can enjoy an active life. The most important intervention for both preventing and treating COPD is not smoking.
Asthma is a common, long-term condition that affects the airways in the lungs. Classic symptoms include breathlessness, tightness in the chest, coughing and wheezing.
Asthma differs from COPD in that restrictions to the airflow are largely reversible, whereas in COPD the restriction is only partially reversible as there is permanent damage to the airways. The goal of treatment for patients with asthma is to be free of symptoms, and able to lead a normal, active life. The causes of asthma are not well understood, so prevention of asthma is not currently possible.
The Barnsley picture and how we compare
Prevalence
Chronic Obstructive Pulmonary Disease (COPD)
- In March 2020, there were 8,658 people on Barnsley COPD primary care QOF registers. This is 3.2% of the GP registered population (60% greater than the English rate of 2.01%).
- The 2016 Respiratory NHS Right Care Pack highlights that lower respiratory tract infections (LRTIs) were twice as high in Barnsley compared to the best five of our comparator CCGs
- Large geographical differences exist within Barnsley, with prevalence rates ranging from 0.8% in Penistone to 4.9% in the Dearne.
Asthma
- In 2019/20, 6.5% of the Barnsley population were recorded on GP registers as suffering with Asthma, the same as the England rate.e 17,247 people
- Compared to 10 similar CCGs, Barnsley’s rate is the lowest.
- Rates have remained fairly constant since 2009/10, with the 2019/20 rate being the highest.
- Geographical variations exist within Barnsley, with prevalence rates ranging from 4.5% to 7.8%.
Smoking prevalence in adults
- Although the proportion of adult smokers in Barnsley has fallen in recent years, the 2019 rate (18.3%) still remains significantly higher than the England average of 13.9%. With higher levels in some localities
Hospital admissions
Emergency hospital admissions for COPD
- Barnsley’s 2019/20 rate for emergency hospital admissions for COPD (882 per 100,000) is significantly higher than the England rate of 415 per 100,000.
- Out of 16 comparator authorities, Barnsley’s rate is the highest.
- The 2019/20 rate is the highest since 2014/15.
- At ward level, only two wards (Penistone East and Penistone West) have lower admission rates than the England average. Rates in St Helens and Stairfoot wards are three times higher than the England average (2013/14 – 2017/18 data).
Hospital admissions for asthma (under 19 years)
- Barnsley’s 2019/20 rate for hospital admissions for asthma in young people aged under 19 (153 per 100,000) is similar to the England rate of 158.3 per 100,000.
- Compared to 10 similar CCGs, Barnsley’s rate is the fifth lowest.
Emergency admissions for children with lower respiratory tract infections
- In 2019/20, Barnsley had a higher rate than England of emergency admissions to hospital for children with lower respiratory tract infections (495.6 per 100,000 compared to 469 per 100,000).
- Rates have fluctuated since 2015/16; the 2019/20 rate of 495.6 is the second highest.
Smoking attributable hospital admissions
- Barnsley’s 2019/20 rate for smoking attributable hospital admissions (2,384 per 100,000) is significantly higher than the England rate of 1,398 per 100,000.
- Out of 16 comparator authorities, Barnsley’s rate is the highest.
- Rates have fluctuated during the period 2015/16 to 2019/20.
Prevention
Flu vaccine uptake (65+ and <65 at risk)
- In 2020/21, 82.6% of adults aged 65+ received the flu vaccine, significantly better than the England rate of 80.9%.
- More than half (57.2%) of those aged under 65 (at risk) were vaccinated, compared to 53.0% nationally.
Smokers that have successfully quit at 4 weeks (CO validated)
- The proportion of smokers in Barnsley who successfully quit at 4 weeks (CO validated) (2,110 per 100,000 smokers aged 16+) is significantly better than the national rate of 1,113 per 100,000. Barnsley’s rate of 2,110 represents 775 smokers who successfully quit at 4 weeks in 2019/20.
Mortality
Under 75 mortality from respiratory disease
- Although Barnsley’s rates for under 75 mortality from respiratory disease have fallen over recent years, the 2017/19 rate of 43.6 per 100,000 is still significantly higher than the England rate of 33.6 per 100,000.
- Compared to similar authorities, Barnsley’s rate is the seventh lowest.
- The rate has reduced from 54.1 per 100,000 in 2001/03.
- At ward level, there are large geographical differences, with rates per 100,000 ranging from 13.8 in Penistone East to 66.6 in Stairfoot. The rates in Dodworth and Penistone East wards are significantly lower than the Barnsley average, whilst the rate in Stairfoot ward is significantly higher.
Under 75 mortality from respiratory disease considered preventable
- In terms of under 75 mortality from respiratory disease that is considered preventable, Barnsley’s 2020 rate of 21.5 per 100,000 is similar to the England rate of 17.1 per 100,000.
- Compared to similar authorities, Barnsley’s rate is the eighth lowest.
- The rate has reduced from 40.5 per 100,000 in 2001.
Data from
- Public Health Outcomes Framework : Indicators 2.14, 4.07i and 4.07ii
- PHE Local Tobacco Control Profiles
- National General Practice Profiles
- PHE Child Health Profiles
- PHE Local Health Profiles
- The Segment Tool
- CCG Outcomes Indicator Set
What we're doing and the assets or services we have
The majority of cases of COPD, asthma and other respiratory disease are managed in the community by primary care and community via SWYPFT . These chronic conditions can worsen suddenly or exacerbate from their usual stable state (or day to day variations), leading to illness that may be acute in onset and may require hospital admission without the right management. Exacerbations are important events in the course of the disease because they can:
- Negatively affect a patient’s quality of life
- Have effects on symptoms and lung function that take several weeks to recover from
- Accelerate the rate of decline of lung function
- Are associated with significant mortality, particularly in those requiring hospitalization
- Have high socioeconomic costs
Avoiding exacerbations is therefore a priority in respiratory care.
COVID-19 will likely have long term implications for respiratory care in the community. Patients recovering from coronavirus will require specialist respiratory input at home eg oxygen support at home, skills focused on admission avoidance and supporting early discharge.
Under 75 mortality from respiratory disease is 30% higher in Barnsley than the national average (2016-2018). This equated to 106 deaths in 2018/19. In 2019, 18.3% of Barnsley’s adult population were smokers, compared to 13.9% for England.
Since 2017, respiratory services in Barnsley have undergone a period of clinical transformation involving significant investment. NHS Barnsley Clinical Commissioning Group (CCG) is working in collaboration with Barnsley Hospital NHS Foundation Trust (BNHFT) and South West Yorkshire Partnership Foundation Trust (SWYPFT) to deliver an integrated respiratory service for patients with COPD/respiratory disease focusing on exacerbation management, diagnosis, pulmonary rehabilitation and ongoing care with the ambition to improve the quality of life of the Barnsley respiratory patient. The established Barnsley REspiratory Assessment and THErapy in The Community (BREATHE) Service aims to improve health outcomes and quality of life for people with COPD/respiratory, and includes Pulmonary Rehabilitation as a key priority.
An increased proportion of patients having acute exacerbations of respiratory disease and respiratory infections are now being supported within the community. Patients who do require emergency admission for an acute /chronic condition will be reviewed by a Specialist Respiratory Nurse within 24 hours of discharge from hospital, 7 days a week. All patients will have a personalised care plan and for those at high risk of exacerbations, home rescue medications.
Primary Care has been enhanced by specialist respiratory multidisciplinary support which will wrap around the locality hubs, providing specialist respiratory advice and interventions such as pulmonary rehabilitation and long term oxygen assessments. This includes a named Respiratory Specialist Nurse aligned to each of the six localities, alongside a series of weekly locality based consultant led Respiratory Clinics, one per locality.
The specialist multidisciplinary respiratory team links closely with the neighbourhood nursing teams and intermediate care services in Barnsley who provide rapid response, hospital at home and general rehabilitation.
All patients with COPD will have a personalised care plan including a flare up plan and for those at high risk of exacerbations, home rescue medications.
An increase in the numbers of people having pulmonary rehabilitation will be achieved, with a particular emphasis on ensuring that many more patients who have been admitted to hospital with an exacerbation of COPD receive the intervention.
Patients enter the service through two main routes, either an Emergency Department (ED) attendance of through their GP or practice nurse referring them into the BREATHE in the Community Service. Patients admitted to hospital are assessed by the BREATHE team then, if appropriate, enrolled onto Early Supported Discharge (ESD) and their condition managed in the community until the exacerbation has resolved.
Opportunities for improvement or future development
My COPD app
To support patients to better manage their condition, the BREATHE in the Community Service has introduced the MyCOPD app. The app is designed to support patients at any stage of the disease. The myCOPD app offers users training techniques for every type of inhaler prescription assessment and identifies if an inhaler medication conflicts with what the patient has been prescribed. It also provides a self-management plan to help patients understand what medication to take and when.
Pulmonary rehabilitation
A range of actions to improve accessibility and reach of the pulmonary rehabilitation service and improve take up rates has been e introduced. Key activities include offering a self-referral route into the service, introducing a home based programme of support to patients and reviewing service delivery locations in line with local health need. People can also be referred to primary care health and well-being coaches for support.
Group consultations peer to peer groups are being introduced and more self-care tools have also been introduced to help people manage their conditions, eg oximetry to monitor oxygen level virtually and weight management support.
Links to Tobacco Control including the QUIT programme.
Resources and supporting documents
Sensory impairment - sight loss
Why this is important
Prevention of sight loss will help people maintain independent lives as far as possible.
Research by the Royal National Institute for Blind People (RNIB) suggests that 50% of cases of blindness and serious sight loss could be prevented if detected and treated in time. Whilst this is mainly due to common eye problems such as uncorrected refractive error and untreated cataract, the research implies that the take-up of sight tests is lower than would be expected. This is particularly the case within areas of social deprivation. Low take-up of sight tests can lead to later detection of preventable conditions and increased sight loss due to late intervention.
Prevention of avoidable sight loss is recognised as a key priority for the World Health Organisation’ (WHO) global initiative for the elimination of avoidable blindness by 2020 - Vision 2020: The Right to Sight, to which the UK is a signatory and which is also a key priority for Vision UK. It is also a particularly important issue in the context of an ageing population.
Risk of sight loss is heavily influenced by health inequalities, including ethnicity, deprivation and age. Sight loss can increase the risk of depression, falls and hip fractures, loss of independence and living in poverty.
The Barnsley picture and how we compare
The Law Commission report (Adult Social Care, May 2011) recommended that local authorities should maintain a register of blind and partially sighted people (Paragraphs 12.15 - 12.18) and this recommendation has been accepted by Department of Health and Social Care Ministers.
Completion of a CVI (certificate of visual impairment) by a consultant ophthalmologist, initiates the process of registration with a local authority and leads to access to services. CVI is a patient choice, and in Barnsley we do not incentivise certification, and services are available to all.
- In 2019/20, the rate for new certifications of visual impairment (CVI) in Barnsley was 61.2 per 100,000. This is significantly higher than the England rate of 41.4 per 100,000.
- Out of 16 similar local authorities, Barnsley’s rate was the second highest.
- In terms of numbers, the rate of 61.2 represents 151 people in Barnsley who were registered as visually impaired in 2019/20.
- Barnsley’s 2019/20 certification rates for preventable sight loss due to age related macular degeneration (AMD) and glaucoma were also significantly higher than the England rates. The rate for preventable sight loss due to diabetic eye disease was similar to the England average.
Data from:
- Public Health Outcomes Framework – indicators E12a, E12b, E12c and E12d.
- Projecting Older People Population Information System (POPPI)
- Projecting Adult Needs and Service Information
What we're doing and the assets or services we have
Our multi-agency Barnsley Vision Strategy Group have a work programme to address prevention of sight loss, support good eye health, and promote independence and social inclusion of those with sight loss. The group have adopted the England Vision Strategy key priorities, refreshed in October 2018; Prevention, Commissioning, Services, Independence, Self Determination, Inclusion.
The group’s work is being informed by engagement work with Barnsley residents with sight loss (adults, children, young people and parents), local services are actively involved in reviewing what is working well, and where there is value in working together. The group have also supported a health needs assessment on preventing sight loss, this report recognises that we still have some work to do to prevent avoidable sight loss in Barnsley, but for those with sight loss our services are working hard to support access to services and CVI (if chosen). The report also provides 20 key recommendations which the Barnsley Vision Strategy Group will be using to inform and develop their work programme moving forward.
Barnsley Vision Strategy Group
The strategy group includes the following:
- Adult service users and parents of children with sight loss
- Commissioners (Barnsley Council and Barnsley Clinical Commissioning Group)
- Primary care services (opticians, GPs, and pharmacies)
- Community services (rehabilitation, sensory, equipment and adaptation)
- Schools and children’s services (Education Inclusion Service)
- Voluntary sector services:
- Barnsley Blind and Partially Sighted Association (BBPSA)
- Royal National Institute of Blind People (RNIB)
- Sheffield Royal Society for the Blind (SRSB)
- Vision Foundation
- Action for Blind People
- Barnsley Healthwatch
- Secondary care services (ophthalmology, eye clinic liaison officer (ECLO), low vision service, diabetic eye screening service)
- National (England Vision Strategy Regional Manager)
The group are aiming to have a strategic action plan for 2020 ready by winter 2019. In the interim, work is ongoing to involve stakeholders, establish links to other local strategies, eg Active in Barnsley, Smoke Free Barnsley, and to develop our local campaign.
Opportunities for improvement or future development
The following Vision Strategy Priorities provide a framework for future developments:
- Prevention - To improve eye health and prevent sight loss across Barnsley within diverse groups and the wider population. Our Health Needs Assessment makes 20 key recommendations for implementation of this.
- Commissioning - To promote effective commissioning strategies across health and social care, supporting an integrated and person-centred pathway. Sharing and reviewing best practice from other local areas, regionally and nationally.
- Services - Adults, children, young people and their families have access to the right services, advice and support when eye health and sight loss problems arise. Services are promoted locally, and Barnsley people know which support to access when a need arises.
- Independence - Adults, children and young people can learn, relearn or retain key life skills on a continuing basis as driven by their needs with access to appropriate professional support, aids and adaptations including technology, and accessible public transport.
- Self-determination - To develop and enable face to face and online peer support opportunities and self-help and self-advocacy resources to empower adults, children, young people and their families to achieve their aspirations.
- Inclusion - To promote inclusive environments and equality of opportunity to enable blind and partially sighted people to fully participate, contribute and live independently.
Resources and supporting documents
Health improvement
This section includes:
- alcohol
- excess weight
- family hub two-year checks
- infant feeding
- physical activity
- school readiness
- sleep
- smoking
- under-18 conceptions
- unintentional and deliberate injuries in children (aged 0 to 4)
Alcohol
Why this is important
Alcohol plays a significant role in our social lives and in our economy: it provides employment, generates tax revenue and stimulates the night-time economy.
Although the majority of people who drink do so moderately, alcohol consumption has doubled over the past 40 years. As a result, alcohol is the leading risk factor for deaths among men and women aged 15–49 years in the UK (PHE, 2018) and there are more than one million alcohol-related hospital admissions every year. The harm from alcohol goes far beyond individual health affecting families, friends and communities; it contributes to violent crime, domestic abuse and absence from work.
The impact of alcohol harm falls disproportionately on the more vulnerable people in society. Those in the lowest socioeconomic groups are more likely to be admitted to hospital or die from an alcohol-related condition compared to those in higher socioeconomic groups, so the action that supports local work to prevent or reduce alcohol-related harm can also help reduce health inequality.
However, it is important that we do not neglect our efforts to those in the higher socioeconomic status groups. A study released by the Office for National Statistics (ONS) has found that the most regular drinkers are those in professional jobs, with 69.5% of professionals reported having drunk in the last week compared with 51.2% of people in routine or manual occupations. Although the relationship between alcohol consumption and socioeconomic status is complex there is a need to dismantle the stereotype around those who are problem drinkers.
The Barnsley picture and how we compare
- Just over a quarter (25.8%) of adults (18+) in Barnsley report drinking over the recommended 14 units of alcohol each week; similar to the England rate of 25.7%.
- The proportion of dependent drinkers in 2016/17 in Barnsley (1.80%) was significantly higher than the national rate of 1.35%.
- Barnsley’s 2018/19 rate for hospital admissions for alcohol-related conditions (856 per 100,000 population) is significantly higher than the England rate of 664 per 100,000.
- The 2018/19 rate of 856 per 100,000 equates to 2,085 hospital admissions of Barnsley residents for conditions that were related to alcohol (1,209 males and 876 females).
- Out of 16 comparator authorities, Barnsley has the fifth highest rate for alcohol-related hospital admissions.
- In terms of younger people, Barnsley’s 2016/17 – 2018/19 rate for hospital admissions in the under 18’s for alcohol-specific conditions for:
- Males (39.0 per 100,000) is similar to the England rate of 25.9 per 100,000.
- Females (67.6 per 100,000) is significantly higher than the England rate of 37.5 per 100,000.
- Under 18 admission rates for males have declined in recent years, from a high of 100.2 in 2008/09 – 2010/11. However, for females, rates have fluctuated, with an increase from 45.7 per 100,000 in 2011/12 – 2013/14.
- In terms of alcohol-related mortality, Barnsley’s 2018 rate of 48.6 per 100,000 is similar to the England rate of 46.5.
- Barnsley’s 2016/18 under 75 mortality rate from alcoholic liver disease (12.3 per 100,000) is significantly higher than the England rate of 8.9 per 100,000, and is the highest since 2004/06.
- Almost half (46.9%) of Barnsley alcohol users in treatment in 2018 left successfully (free of alcohol dependence) and did not re-present for treatment within 6 months. This is significantly better than the England rate of 37.6% and a significant improvement from the 2010 rate of 17.0%.
Data from:
- Public Health England (PHE) – Local Alcohol profiles for England - the Local Alcohol Profiles for England tool allows you to compare local authorities and compare against the England or regional average.
- Public Health England (PHE) Liver Disease Profiles
- Alcohol dependence prevalence in England - GOV.UK
What we're doing and the assets or services we have
Alcohol is one of three priorities in the refreshed Public Health Strategy along with food and emotional resilience.
To ensure we have a good understanding of alcohol demographics, alcohol-related harm, alcohol treatment and what our partners are already doing in this area, Barnsley Council Public Health team decided to complete the alcohol CLeaR (Challenge, Leadership, Results) assessment tool.
The alcohol CLeaR self-assessment tool has been produced by Public Health England (PHE) to support an evidence-based response to preventing and reducing alcohol-related harm at a local level and builds on experience and successes from the tobacco control CLeaR model.
CLeaR helps place-based alcohol partnerships to assess local arrangements and delivery plans providing assurance that resources are being invested in a range of services and interventions that meet local need and which, the evidence indicates, support the most positive outcomes.
The CLeaR self and peer-assessment have been completed in Barnsley and 40 areas of improvement have been identified.
Our alcohol plan
Based on results from the CLeaR assessments, an alcohol plan has been developed that sets out the priorities and suggested outcomes for addressing alcohol-related harm in Barnsley. We have identified six priorities:
- night time economy
- availability
- affordability
- acceptability
- children and young people
- partnership approach
- alcohol treatment
A high-level detailed alcohol action plan has also been developed to ensure we are working towards each priority area and our progress is measured.
In addition to the work already mentioned, Barnsley Council’s Public Health team have formed an Alcohol Alliance. The overarching purpose of the Barnsley Alcohol Alliance is to develop a system-wide approach to address the availability, affordability and acceptability of alcohol in Barnsley. This Alliance brings together a wide range of partners with the aim of working together to implement, manage and evaluate the alcohol plan, alcohol improvement plan and a range of alcohol-related targets. The Barnsley Alcohol Alliance will provide a shared voice, leadership and a joint opportunity for all its members in a way that allows us to do more together than could be achieved by acting in isolation.
An area that we have been working on over the last two years related to alcohol, and also assisting with cross Council priorities, is that of the Night-Time Economy (NTE). This work is continuing and is focused on:
- An award-winning Best Bar None scheme in the town centre. A good proportion of town centre bars and clubs are now signed up to the scheme and due to a new BBN category of ‘Best Dining Experience’ some restaurants have now also been accredited with the award.
- A Night Life Marshal service that ensures that the taxi queues are well managed and vulnerable people due to intoxication are kept safe.
- Security Industry Accreditation training events for all NTE staff, which may include: door staff, licensees, Marshals and street pastors and bar staff.
- An Ask for Angela scheme that all BBN Venues are signed up to.
Barnsley town centre continues to set itself apart from other areas having been awarded with prestigious Purple Flag status. This identifies the town centre as offering an entertaining, diverse, safe and enjoyable night out. Barnsley joins only three other towns in the Yorkshire region to gain Purple Flag Status; those include Leeds, Sheffield and Halifax.
The Purple Flag standard is an accreditation process similar to the Green Flag award for parks and the Blue Flag for beaches. It allows members of the public to quickly identify town & city centre’s that offer an entertaining, diverse, safe and enjoyable NTE.
The Purple Flag has a number of benefits for towns, with the associated raised profile and public image contributing to increased expenditure and lower crime and anti-social behaviour.
The accreditation was achieved thanks to a number of measures put in place by Barnsley Council, including tackling binge drinking
Opportunities for improvement or future development
Improvements to the availability, affordability and acceptability of alcohol in Barnsley, in addition to the other four priorities of the alcohol plan, will be made by keeping track of the Alcohol Action Plan and support from the Alcohol Alliance.
A collaborative approach to understanding the local data via an in-depth analysis will also be initiated. The exceptionally high rates of alcohol-specific hospital admission episodes for females under the age of 18 have been highlighted as a particular focus area to investigate. Consequently, we are working closely with Barnsley District General Hospital to complete a retrospective case review. Through completion of this, we will acquire a greater understanding of the circumstances of individual cases, identifying the journey that patients go through prior, during and following an alcohol-specific hospital admission. With this knowledge, we will be better equipped to generate effective targeted intervention and reduce the aforementioned admission rates across the borough.
The aim for the next 12 months is to work towards maintaining our Purple Flag flag. We will also strengthen the Alcohol Alliance by ensuring the right people are in attendance and build good working relationships with those involved in the Alcohol Action Plan. We will continue with our communications approach around alcohol-related harm and link with our partners so as a borough, we are sending out consistent evidence-based messages.
Excess weight
Why this is important
Healthy eating helps us to maintain a healthy weight and reduces our risk of type 2 diabetes, high blood pressure, high cholesterol and the risk of developing cardiovascular disease and some cancers such as breast, bowel and pancreatic cancer. Healthy eating also has many other benefits. When we eat well, we sleep better, we have more energy and better concentration levels.
Overweight and obese children are becoming bigger at an earlier age and are staying obese into adulthood. It is estimated that obesity is responsible for more than 30,000 deaths each year. On average, obesity deprives an individual of an extra 9 years of life, preventing many individuals from reaching retirement age. Cancer Research UK has predicted that in the future, obesity could overtake tobacco smoking as the biggest cause of preventable death. Obesity increases the risk of developing a range of diseases. Obese people are:
- at increased risk of certain cancers, including being 3 times more likely to develop colon cancer
- more than 2.5 times more likely to develop high blood pressure - a risk factor for heart disease
- 5 times more likely to develop type 2 diabetes
The economic cost for obesity is worryingly high and is having an impact on economic development and the NHS. The overall cost of obesity to wider society is estimated at £27 billion. The UK-wide NHS costs attributable to overweight and obesity are projected to reach £9.7 billion by 2050, with wider costs to society estimated to reach £49.9 billion per year.
Local Barnsley rates of adult excess weight (overweight and obese combined) are 65.8% which is similar to the national average of 62.3% (PHE, 2108/19).
Source: Public Health England
The Barnsley picture and how we compare
Adults:
- Latest data (2019/20) indicates that almost three-quarters (73%) of Barnsley adults are overweight or obese; a significantly higher proportion than the national average (62.8%).
- Out of 16 similar local authorities, Barnsley’s rate is the third highest.
- Almost three out of ten Barnsley mothers (28.9%) in 2018/19 were classified as obese at the time of their maternity booking appointment; a significantly higher proportion than the national average of 22.1%.
Children:
4-5 year olds:
- Almost one in five (19.4%) of Barnsley’s 4-5 year old population were overweight or obese (excess weight) in 2019/20*; a significantly lower proportion than the England rate of 23.0%.
- Out of 15 similar local authorities, Barnsley’s 2019/20 rate was the lowest.
- Excess weight in 4-5 year olds in Barnsley has fluctuated in recent years (from a high of 23.6% in 2015/16).
- At ward level, excess weight rates range from 10.7% in Darton East ward to 30.4% in Worsbrough (three years aggregated data (2017/18-2019/20).
10-11 year olds:
- A third (33.4%) of Barnsley’s 10-11 year olds were overweight or obese in 2019/20*; similar to the England rate of 35.2%.
- Out of 16 similar local authorities, Barnsley’s 2019/20 rate was the lowest.
- Excess weight in 10-11 year olds in Barnsley has fluctuated in recent years (from a high of 35.6% in 2006/07).
- At ward level, rates range from 25.0% in Penistone East ward to 40.0% in Central ward (three years aggregated data (2017/18-2019/20).
* The 2019/20 NCMP data collection stopped in March 2020 when schools were closed due to the Covid-19 pandemic. In a usual NCMP collection year, national participation rates are around 95% (over a million) of all eligible children, however in 2019/20 the number of children measured was around 75% of previous years. Despite the lower than usual number of measurements, analysis by NHS Digital indicates that figures at national and regional level are directly comparable to previous years, for all breakdowns.
Data from:
-
Public Health Outcomes Framework – indicators C03a, C09a, C09b and C16
- National Child Measurement Programme
What we're doing and the assets or services we have
- Barnsley Clinical Commissioning Group (CCG) commissions the tier 3 weight management service for children and adults.
- The Good Food Barnsley Partnership is a network of voluntary and statutory partners with the vision to build a better Barnsley, where everyone has the right to access the food they need to thrive. The partnership works on initiatives that tackle food poverty and improve the nutritional knowledge and cooking skills of the community.
- Development and promotion of a ‘pilot’ Wellbeing Service, which incorporates two elements – Grants to local area teams to promote mental and physical wellbeing, as well as a Wellbeing Support Programme (GP referral) delivered by Barnsley Premier Leisure, a scheme offering 1:1 & group support for individuals wanting to change behaviour, improve levels of activity, diet, nutrition and wellbeing.
- The 0-19 Public Health Nursing Service support overweight and obese children and families as identified through the National Childhood Measurement Programme.
- The Local Plan was adopted in Spring 2019. Through our planning processes, we are limiting the growth of additional hot food takeaways across the borough. Planning applications will consider the childhood obesity rates when reviewing applications. Applicants are now asked to complete a health needs assessment, and rules have been introduced about the number of hot food takeaways on one front to prevent over concentration in areas.
- We work closely with school catering teams in the development of new and existing menus so that children across Barnsley have access to hot nutritious and enjoyable school meals throughout the school week. We use local and regional produce to reduce food miles and maintain a local supply chain and are accredited with both Chartered Institute of Environmental Health (CIEH) and Royal Society of Public Health (RSPH).
- Advertising of High Fat, Sugar and Salt (HFSS) products. We know that exposure to advertising influences what food and drink products we choose to consume, especially amongst children. Working with local and regional partners, we will restrict the advertisement of HFSS products, whilst promoting the advertisement of healthier options, especially where children are more exposed to the advertising (eg near to schools).
Opportunities for improvement or future development
The Barnsley Food Plan 2018-21
The food plan will require partnership delivery which will address issues around healthy weight, but it is not limited to that alone. The plan is about changing the food environment and culture within Barnsley, as well as improving access to quality food and improving health and wellbeing outcomes. Our approach will focus on developments to the policies and structures which we live, work, shop, eat and learn within. Barnsley’s food plan has been developed in response to priorities in the 2018 refreshed public health strategy and will help to influence the social, cultural and environmental conditions around us. The plan will prioritise local supply chain, the reduction of sugar, education, public sector catering, the consumer food environment and food access.
The plan aims to achieve a number of outcomes specifically relates to its priorities.
- Supply chain: We will celebrate the food journey from production to waste.
- Consumer environment: Food will play a key role in strengthening our local economy and connections with our businesses and communities.
- Sugar: We will reduce the amount and frequency consumed by our children and young people.
- Education: Residents and employees will have an improved understanding of the importance of a healthy balanced diet.
- Public sector catering: We will be exemplar and serve quality products.
- Access: Each person will have access to food that is nutritious, affordable, diverse and that benefits their health and wellbeing.
Resources and supporting documents
Family hub two-year checks
Why this is important
The two-year progress check is the first statutory assessment point in the Early Years Foundation Stage.
Analysis of the borough wide data enables services to plan and work together, in order to address areas of learning where attainment is low. The analysis derived from the borough’s two-year progress checks is shared widely and is used to inform family hub delivery of services, for example outreach priorities for stay and play/parent and child groups. The data is also shared with primary schools to support effective transition and to enable schools to better meet children’s needs from the outset, ultimately improving outcomes at the end of the Foundation Stage (second statutory assessment point).
The data has been used when working on government initiatives as part of the social mobility agenda. The main focus for this work has direct links to the two year data for the borough and has a focus on improving communication and language.
The Barnsley picture and how we compare
- Within Barnsley, rates for two year olds achieving typical or above typical development range from 43.5% in the health and self care aspect to 70.6% in the moving and handling aspect.
- Girls perform better than boys for every aspect within the personal, social and emotional development area, the physical development area and the communication and language area.
- Non-funded two year olds perform better than funded for all aspects within each area (personal, social and emotional development, physical development and communication and language).
Resources and supporting documents
Infant feeding
Why this is important
On average there are around 2,500 births each year in Barnsley. Most women are aged between 20 to 34 years when they give birth.
Maternal behaviours such as diet, smoking, drug and alcohol use, breastfeeding and maternal weight have an impact on the health and wellbeing of both the mother and baby. Breastfeeding saves lives, protecting the health of babies and mothers immediately and over time. It reduces the risk of Sudden Infant Death (SID) and babies who are breastfed are less likely to develop infections. Longer term benefits of breast milk include a reduced risk of becoming obese, developing diabetes, high blood pressure and high cholesterol levels. For mothers there is a decreased risk of breast and ovarian cancers and heart disease in later life. It also supports the mother-baby relationship fosters strong positive attachment which protects the mental health of both baby and mother beyond the early years.
In Barnsley just over half of women start breastfeeding their baby, this falls to around a third of women breastfeeding when their baby is 6-8 weeks old. As well as health values to mother and baby, increased breastfeeding rates contribute to reducing health inequalities through improved outcomes. Financially, high rates of breastfeeding not only result in savings to family budgets, but also to reduced service costs associated with dealing with health problems which occur more frequently when babies are not breast fed.
Although breastfeeding is the optimal choice for mums, babies and our environment and the Infant Feeding Team work to support mothers to breastfeed, they also work to ensure that all babies receive high standards of care and the best possible chance to thrive regardless of feeding type.
The Barnsley picture and how we compare
- Under half (47.4%) of mothers in Barnsley in 2018/19 gave their babies breast milk for their first feed. This is significantly lower than the England rate of 67.4%.
- Out of 16 comparator authorities, Barnsley’s rate is the lowest.
- There are large variations in the proportion of mothers in Barnsley who initiate breastfeeding, with rates ranging from 37.1% in Dearne North ward to 72.5% in Penistone East ward (2016/17 - 2018/19 data).
- A third of mothers in Barnsley (33.3%) continue to breastfeed their babies at 6-8 weeks after birth; significantly lower than the national rate of 47.6%.
What we're doing and the assets or services we have
Barnsley Maternity Services (provided by Barnsley Hospital NHS Foundation Trust) and the 0-19 Public Health Nursing Service (PHNS; provided by Barnsley Council) work together to provide integrated breastfeeding support. The PHNS also includes a dedicated Infant Feeding Team to ensure women and their partners/supporters are fully informed and empowered to initiate and continue breastfeeding for as long as they choose and are able to access timely and appropriate support when queries arise.
We have strong multiagency working across all partners and to support this we have in place a multi-agency Maternal and Infant Feeding Implementer Group chaired by a Public Health Senior Practitioner who is the designated strategic lead for infant feeding.
Barnsley Hospital and Barnsley Council’s 0-19 Public Health Nursing Service (PHNS), Family hubs and infant feeding staff have all been Baby Friendly Initiative UK (BFI) accredited since 2010 and were reaccredited in December 2019. Implementing the BFI standards provides effective professional support to mothers and their families (PHE recommendation).
We comply with WHO International Code of Marketing Breastmilk Substitutes by restricting the advertising of breastmilk substitutes including formula milks, baby foods (before 6 months), bottles and teats.
Our Director of Public Health, Julia Burrows is a Baby Friendly Initiative Guardian. This role has the responsibility of promoting, protecting, supporting and normalising breastfeeding supported by the Baby Friendly standards, including compliance with the International Code of Marketing of Breastmilk Substitutes.
There is a joint borough wide Infant Feeding Policy with related pathways and guidelines in place.
The PHNS Infant Feeding Team includes both paid and voluntary staff who provide mother to mother peer breast feeding support via antenatal and postnatal discussions on infant feeding, telephone triage and one-to-one contact at virtual breastfeeding groups or via home visits and via social media ie Facebook and Instant Messenger. The service also provide support for mothers with multiples and breastfeeding management challenges.
In response to the Covid-19 lockdown, the PHNS Infant Feeding Team developed a closed Facebook group to provide virtual peer-to-peer support for breastfeeding mums across Barnsley to share their experiences with one another and also to support them with sharing their experiences with breastfeeding / needing support with breastfeeding.
Pre-pandemic, breastfeeding peer support training was provided in local communities to improve community capacity. Unfortunately, due to the current climate we have been unable to deliver any peer support training. However, the service continue to work with and develop volunteers wherever possible. There are currently 5 active infant feeding volunteers, 2 working at Barnsley Hospital on the maternity wards and 3 facilitating the closed social media group. A closed group has also been set up through Facebook for all those who have completed peer support training.
The PHNS Infant Feeding Team also run an antenatal course via social media providing antenatal information over a 2 week period. This course has evaluated very well and families where English is not the first language have used the Google translate facility which has enabled us to meet their requirements better. We also use the Unicef Baby Friendly resources which provides different languages.
Where possible face-to-face support is provided however, as face-to-face contact was reduced during the Covid-19 lockdown the PHNS Infant Feeding Team have started using video conferencing to enable observation of a feed, where the mother is willing.
A free breast pump loan scheme is in place, with premature, ill babies and mothers given priority.
Our Breastfeeding Welcome Here Scheme is in place to ensure all families should be able to breastfeed their babies in public places without fear of harassment or discrimination. The Equality Act 2010 has specifically clarified that it is unlawful for a anyone to discriminate against a woman because she is breastfeeding a child.
We have a communications and digital offer with websites with links to Family hubs, maternity websites and a Facebook page. This supports wider initiatives and opportunities such as use of family hubs, Stop Smoking Service, libraries and foodbanks.
The service promotes local, national and world-wide events such as World Breastfeeding Week and other initiatives.
The Unicef UK BFI mandatory infant feeding training for multiagency staff has been redeveloped into a virtual offer by the Infant Feeding Lead at Barnsley Hospital and the PHNS Infant Feeding Team Leader.
All 7 PHNS Infant Feeding Support Workers have attended BFI training on Breastfeeding and Building Relationships in 2021 as well as 2 members of staff from the wider service.
Barnsley are part of the Yorkshire and Humber Climate Change Sub Group who have submitted an abstract for the SLI Conference. As part of COP26 a lite bite event was delivered across the whole of the Council by PHNS Infant Feeding Team to demonstrate the value of breastfeeding for our environment.
Healthy Start
Healthy Start is a government welfare food scheme. Healthy Start supports young and low income pregnant women and families with children under the age of four years in the UK by providing monetary vouchers, vitamins, nutritional and breastfeeding information.
Barnsley Council commissions a free two months supply of vitamins for all pregnant women at their first appointment, for infants who are breastfed and when infants reach eight to twelve months of age.
Pregnant women who are not-eligible for the Health Start scheme can purchase vitamins at a reduced rate from the family hubs.
Opportunities for improvement or future development
Barnsley Leading the Way - We have been asked by the Yorkshire and Humber section of the National Infant Feeding Network to share 'How It Works' around our antenatal Facebook group.
Face-to-face Antenatal Workshops
Pre-pandemic face-to-face antenatal workshops at Barnsley Hospital were being piloted with positive feedback but these were stopped due to the Covid-19 lockdown. Future consideration will be given to the restarting of these workshops once it is safe to do so.
Face-to-face peer support groups
Pre-pandemic there were face-to-face peer support groups in each of the Barnsley localities, facilitated by a member of the PHNS Infant Feeding Team. These were stopped due to the Covid-19 lockdown and a virtual offer developed. The service is currently considering a new hybrid offer with both virtual and face-to-face support available in the community.
Specialist services
We are keen to develop and improve services for breastfeeding mothers with more specialist challenges. A business plan is currently being developed for a Midwifery led Tongue Tie Service, with the aim of holding a couple of clinics a month at Barnsley Hospital. Future work is to develop training for healthcare practitioners in identifying tongue tie and improving the referral process and pathway.
Return to work and study
We are working to provide improved support to employers to implement policies, practices and environments that support mothers to breastfeed during study and work. The breastfeeding welcome and breast pump loan scheme already support women with the transition of returning to work. Work is ongoing with BMBC to improve the Maternity Policy such that more women are supported to breastfeed on their return to work in the Council. BMBC family hubs have offered BMBC employees as well as Midwifery staff to use their facilities to breastfeed, whilst working out in the community.
Volunteer peer support training
We are eager to support and improve the uptake of infant feeding volunteers across the borough. A future aim is to develop online peer support training.
Incentives schemes
We are considering the opportunities which an incentive scheme may bring in an effort to improve breastfeeding rates. This is based on the outcomes of The Nourishing Start for Health (NOSH) study which showed an increase in breastfeeding in the areas where it was offered.
Healthy Start vitamin remodel
The current Healthy Start vitamin scheme is under review and a new model of provision is in development to ensure that the families who need the vitamins most have access to them.
Neonatal Unit
Barnsley Hospital’s Neonatal Unit has recently received funding to apply for BFI accreditation.
GP updates
Infant feeding updates for GP’s are currently being explored to support them in promoting, supporting and protecting breastfeeding in their practices.
Cultural competence self-assessment
This will be completed across Maternity and PHNS, to identify areas which may need to be strengthened to ensure that all families receive infant feeding support that is culturally relevant and appropriate to them.
BFI reaccreditation
BMBC and Barnsley Hospital are due for BFI reaccreditation in December 2022. Following this, the aim is to go for the Achieving Sustainability ‘Gold’ award.
Resources needed for future development
Funding opportunities need to be sought to deliver our suggestions for future improvements and developments.
Resources and supporting documents
- Public Health Outcomes Framework – indicators CO5b
- Public Health England (Child Health Profiles)
- Child and Maternal Health Intelligence Network (CHiMAT)
- The Healthy Child Programme (HCP) - aims to increase rates of breastfeeding initiation and continuation, which will contribute specifically to improving breastfeeding and obesity outcomes.
- UNICEF UK – The Baby Friendly Initiative
- NHS Long Term Plan recommends UNICEF UK Baby Friendly accreditation across all maternity services and includes a focus on improved support for families with infants in neonatal care.
Physical activity
Why this is important
Physical activity includes any form of movement which raises the heart rate and has a positive impact on mental and physical wellbeing. It can include daily living tasks such as housework and gardening, transport such as cycling, walking and scooting, as well as more organised activities such as using the gym, park run or playing team sport.
The benefits of being physically active are well established. Regular participation in physical activity can reduce the risk of many chronic conditions including coronary heart disease (CHD), type 2 diabetes, cancer, stroke, obesity, mental health illness and musculoskeletal conditions. Physical activity helps by strengthen the heart, lungs and bones, improving our mood and reducing anxiety.
Being active can have a hugely positive impact on individual’s health. Deprived communities generally have a lower life expectancy and a lower healthy life expectancy. By increasing physical activity levels, we can reduce these health inequalities enabling more people to enjoy good health for longer. Importantly physical activity improves our quality of life through immediate and long term benefits.
The Barnsley picture and how we compare
Physically active:
-
Latest data (2019/20) indicates that less than two-thirds (62.7%) of Barnsley adults are physically active (doing at least 150 minutes physical activity per week). This is similar to the England rate of 66.4%.
-
Out of 16 similar local authorities, Barnsley’s rate is the eighth highest
-
The rate in 2019/20 is lower than the 2018/19 rate of 64.3%, but is the second highest since 2015/16, when it was 59.7%.
-
- In 2018/19, 46.1% of Barnsley children and young people (aged 5-16) were physically active (undertaking an average of at least 60 minutes of physical activity per day). This is an increase from the 2017/18 rate of 36.9%.
-
Out of 16 local authorities, Barnsley’s rate is the sixth highest.
Physically inactive:
- Latest data (2019/20) indicates that more than a quarter (28.7%) of Barnsley adults are physically inactive (doing less than 30 minutes physical activity per week). This is significantly worse than the national rate of 22.9%.
- Out of 16 similar local authorities, Barnsley’s rate is the fifth highest.
- The 2019/20 rate is the highest since 2015/16.
Walking
- The proportion of adults in Barnsley that walk (continuously for over 10 minutes) at least five times a week (28.2%) is lower than regional and national rates of 31.4% and 32.7%. However, the 2018/19 rate of 28.2% is higher than the 2015/16 rate of 26.8%.
- 16.7% of adults in Barnsley walk for leisure at least five times a week; similar to the regional and national rates of 17.1% and 16.7%, and an increase from the 2015/16 rate of 15.5%.
- A third of adults (34.5%) in Barnsley walk for travel at least once a week; lower than the regional and national rates of 39.3% and 42.1%. However, the rate is higher than it was in 2015/16 (31.9%).
Cycling
- The proportion of adults in Barnsley that cycle (for any duration) at least once a week (5.7%) is lower than regional and national rates of 9.7% and 11.2%. However, the 2018/19 rate of 5.7% is higher than the 2015/16 rate of 4.0%.
- 5% of adults in Barnsley cycle for leisure at least once a week; lower than the regional and national rates of 7% and 7.6%, but an increase from the 2015/16 rate of 3.7%.
- 2.4% of adults in Barnsley cycle for travel at least once a week; lower than the regional and national rates of 4.4% and 5.9%. However, the rate is higher than it was in 2015/16 (1.9%).
What we're doing and the assets or services we have
Active in Barnsley – Physical Activity Strategic Plan (2018 to 2021)
The Physical Activity Strategic Plan sets out the priorities for getting Barnsley more physically active and will inform the Public Health Strategy 2018-21. Ensuring that all Barnsley residents have the opportunity to benefit from being more physically active. To achieve the vision of a
“healthy and proud Barnsley where active living is part of everyday life for everyone”
we have identified 5 priorities:
- Active Schools and Colleges
- Active Workplaces
- Active Spaces
- Active Communities
- Professional and Volunteer Networks
To experience the many benefits of a physically active population, the Active in Barnsley partnership recognise the need to work collaboratively to create a borough that is designed around healthy, happy and active living for all.
An implementation plan and a communications plan will be created by August 2019 that will drive the work of the Active in Barnsley partnership forward.
Active Travel Strategy (2019 to 2024)
The Barnsley Active Travel Strategy is designed to build upon Barnsley Metropolitan Borough Council’s (BMBC) vision of promoting walking and cycling and encouraging active travel in Barnsley. The vision for active travel is set out in the Barnsley Active Travel Strategy and includes the following:
“Creating a borough where active travel is a preferred choice, supported by a connected network of high quality, safe and inviting cycle routes and footpaths for all people to use”
Delivering this vision will lead to more people walking and cycling and contribute to the following outcomes:
- Improved health and reduced health inequalities by introducing active travel into everyday life;
- Increased economic growth and productivity leading to higher living standards;
- Reduced congestion on the highway network by providing better travel choices;
- Improved Air Quality;
- Safer Active Travel Routes.
These outcomes will be realised by delivering the following actions:
-
Integrate active travel into the planning process
The Barnsley Active Travel Strategy will ensure active travel is prioritised in future planning processes. In addition, it will encourage active travel to be better integrated with other types of transport, eg walking to the bus stop or cycling to the train station. - Provide and maintain active travel routes
Barnsley needs purpose fit active travel routes that people want to use. Barnsley’s existing walking and cycling routes have been developed over time as resources have allowed. They are not always continuous or direct, and may not serve important areas of interest, which means that some people who would like to actively travel are unable to do so. It is important that these routes are well maintained and designed to be as inclusive as possible. - Support active travel in the community
There is a need to encourage and promote active travel in our community. People need the skills, confidence, correct information and most importantly the motivation to make active travel a preferred choice. Initiatives to support this change include pedestrian and cycle training, road safety campaigns, projects to encourage active travel to schools and employment and promotion and advertisement of available routes.An implementation plan will be created by August 2019.
- GP exercise referral scheme
This is delivered by Barnsley Premier Leisure (BPL) and is defined as the Health Referral Scheme where GPs can refer or patients can self-refer if they fit the eligibility criteria. This is one of the elements of a wider offer to support increased physical activity and weight management. This service has been developed by BPL to complement and add value to their physical activity offer. There is a small charge for the service to make it more sustainable.
Commissioned services supporting target groups
Wellbeing Service
The Barnsley Wellbeing Service has two strands;
- BPL wellbeing support programme
- Area Wellbeing Grants
Wellbeing Support Programme
Barnsley Premier Leisure (BPL) will deliver one element of the new Wellbeing Service that offers specialist support to people (one to one or group) who are motivated to change their lifestyle by becoming more active, connected, learning, giving and taking notice (Five Ways to Wellbeing Framework).
The service is GP referral only and offers will provide an eight to 12 weeks Wellbeing Support Programme to address mental wellbeing, physical activity and diet/nutrition. This offers an extension to the existing health referral programme to include diet and weight management support for people who require additional help to make sustainable lifestyle change. It is also important to ensure that this support is aligned with existing local provision/groups working closely within local area teams/ward alliances to ensure integration and sustainability within the community to ensure people are empowered and enable to help themselves in future.
Wellbeing Grants
Area Teams have also been allocated wellbeing grants to offer/extend/add value to community-based services/groups/initiatives, targeting those who cannot or do not engage with services to improve their mental and physical health and wellbeing. These funds have been allocated based on Index of Multiple Deprivation (IMD) and the number of Lower Super Output Areas (LSOAs) in each locality to ensure funding was fairly distributed to the most disadvantage areas. The grants support the outcomes of the Five Ways to Wellbeing; Be Active, Connect, Give, Take notice, Keep learning.
To date, most of the grants have now been allocated – with some area teams offering a second round. A range of the grants have been offered to support physical activity, but the themes are broad ranging.
Live Well Barnsley, area councils and physical activity
Live Well Barnsley is a directory of services for the whole of Barnsley, offering an overview of activities, groups, one-off events, services and peer support across a range of different issues and areas. The website was contracted out, but has now been brought in-house to BMBC and is in the process of being re-built to enable easier navigation and regular maintenance to ensure the content is up to date.
This does encompass some of the information and services commissioned by Area Councils, and creates opportunities for other commissioned services to signpost customers to local services and support available in their area.
Commissioned Activation Programmes
Working with local partners and with Sport England, Barnsley is currently delivering two targeted projects:
- Active Dearne
This is funded through the Tackling Inactivity Economic Disadvantage (TIED) fund and is an exciting programme to support adults and families on low working incomes across the Dearne Valley to become more active. For Barnsley this is specifically the Goldthorpe and Thurnscoe communities in the first year (2019) with the addition of Bolton Upon Dearne in the second year (2020). - Families Fund
This is funded by the Sport England Families Fund over three years (2019-2021) and provides physical activities opportunities to families who have been identified as requiring support. The programme is delivered by Barnsley Council’s 0-19 team and is gradually being rolled out across all family hubs in the borough.
NHS Get Fit First Programme
The NHS Health and Wellbeing programme aims to make sure that people are in the best possible health, and are able to recover better, following a routine, non-urgent operation.
This is for people who have a body mass index (BMI) of 30 or over or who are a smoker. People on the programme will be encouraged to attend a weight management service or a stop smoking service. Support is provided to lose weight or quit smoking, to improve health, reduce risks and to become healthy before and stay healthy after their operation.
Places to play, enjoy and be active
Barnsley is working hard to ensure that our parks, open spaces, playing facilities, leisure centres, golf courses and off road cycling and walking network is promoted and maintained to a level that encourages people to utilise these spaces for formal, informal and recreational use. These include:
- Parks
- Playgrounds
- Golf Courses
- Leisure Centres operated by Barnsley Premier Leisure
- Trans Pennine Trail and National Cycling Network
- Country Parks
Opportunities for improvement or future development
We will be building on whole system planning for implementing our Active in Barnsley partnership to enable local people to move more. This will involve working with a wider range of stakeholders including planners and developers, public transport operators, health care organisations, the leisure industry, community and voluntary sector and residents.
We want to further engage businesses and organisations to improve opportunities for staff wellbeing, particularly to moving more and travelling more actively.
We will be working with local healthcare organisations to ensure physical activity is consistently included within primary and secondary care consultations and patient pathways.
Resources and supporting documents
- Public Health Outcomes Framework – indicators C17a and C17b
- Public Health England NCMP and Child and Maternal Health Profile
- Sport England (Active Lives Survey)
- Walking and cycling statistics: England 2018
School readiness
Why this is important
School readiness starts at birth with the support of parents and caregivers, when young children acquire the social and emotional skills, knowledge and attitudes necessary for success in school and life.
Ages 4 to 5
Between the ages of four and five, children should:
- Be prepared to be separated from their parent or main carer.
- Be able to clearly demonstrate their ability to listen and follow age appropriate instructions.
- Show an interest in a variety of subjects, paying attention to the subject or activity they are taking part in.
- Have a range of vocabulary and language to be able to express their needs, feelings, thoughts or ideas.
- Be able to identify themselves by name, age, and state factors in their life eg name family members.
- Be able to interact in an age appropriate way with another child or adult.
- Be able to interact, share and play, taking responsibility for their actions and understanding repercussions for their actions.
- Be able to focus on and also show interest in the work they are undertaking.
- Be able to observe, notice, discuss and ask questions about their environment and experiences.
- Be able to engage with books and have some understanding of words and language.
- Respond to boundary setting.
- Be able to vocalise their needs such as toileting, thirst, hunger, illness etc.
- Be able to engage in age appropriate fine motor skills and the ability to care for themselves in dressing, toileting and eating and drinking.
Age 5
School readiness at age five is important because it has a strong impact on future educational attainment and life chances. Children who don’t achieve a good level of development aged five years struggle with social skills, reading, maths and physical skills, which impacts on outcomes and in childhood and later life including: educational outcomes, crime and health. Children from poorer backgrounds are more at risk of poorer development and the evidence shows that differences by social background emerge early in life.
The return on investment is greater than many other economic development options:
- For every £1 spent on early years education, £7 has to be spent to have the same impact in adolescence.
- The benefits associated with the introduction of the literacy hour in the UK outstrip the costs by a ratio of between 27:1 and 70:1.
- Targeted parenting programmes to prevent conduct disorders pay back £8 over six years for every £1 invested with savings to the NHS, education and criminal justice system.
The School Readiness outcome indicator is defined as “children who have reached a good level of development at the end of the Early Years Foundation Stage (EYFS) as a percentage of all eligible children in Barnsley.
Children are defined as having reached a good level of development if they achieve at least the expected level in the early learning goals in the prime areas of learning (personal, social and emotional development; physical development; and communication and language) and the early learning goals in the specific areas of mathematics and literacy.”
The Barnsley picture and how we compare
- In 2017/18, 70% of five year olds in Barnsley achieved a good level of development at the end of Reception; similar to the England rate of 71.5%.
- When compared to similar local authorities, Barnsley’s rate was ranked 6th out of 11 (where 1 is the best).
- Rates have been increasing over recent years, and the 2017/18 rate is significantly higher than it was in 2012/13.
- 4% of children had the Ages and Stages Questionnaire (ASQ-3) completed as part of their 2-2 ½ integrated review (2017/18).
Data from:
What we're doing and the assets or services we have
0-19 Team
The 0-19 Public Health Nursing Service delivers the Healthy Child Programme across Barnsley and getting ready for school is one of the six high impact areas of the programme. The service is mandated to provide five health reviews – antenatal health promoting visit, new baby visit, 6-8 week assessment, 9-12 month review and 2-2 ½ review which is undertaken jointly with early years settings personnel.
For children who are in a childcare setting, termly contact with the child’s key worker assesses school readiness. For children who are not in a childcare setting, a targeted assessment is undertaken in line with the service’s school readiness care pathway. Where a need is identified, children are put on the relevant care pathway, such as, toileting, behaviour, development delay.
Family hubs
Educational programmes and projects
Family hubs deliver the antenatal education programme called having a baby. The programme was developed as a multi-agency approach in partnership with Barnsley family hubs and health professionals to support families to adapt to parenthood. This is delivered by staff from children’s centres, midwives, the infant feeding team and health visitors, the Having a Baby programme helps make significant improvements to people’s lives, giving Barnsley babies the best possible start in life and supporting parents with practical information and advice.
The Dearne Family hubs have recently launched a project called Little Talkers, targeting children aged 12-18 months for phase 1 of the initiative. Staff will work with parents in the home to support speech and language by delivering activities and reading stories to support parents’ understanding of different ways to engage with their child it the home. Resource packs will also be used with the family. Staff re-visit the family after six months to see if progress has been made and if the intervention has made a difference.
Toddler groups
The family hubs also run baby and toddler groups to support parents with activities and share the benefits of play and interaction. The groups have a planned learning intention which have primary focuses on Personal Social and Emotional Development (PSED) and Communication to support parents to learn the benefits of play and interaction with their child.
Day care
A number of the family hubs have day-care on site with fully qualified staff who work with children to prepare them for school. A plan is put in place for individual children’s needs with regards to starting school and stages of development. Staff regularly meet with parents and provide them with additional activities and next steps so they can be supported to get their children ready for school at home.
Nurseries
Nurseries also include activities that aim to get children ready for school including
- Role play areas with school uniform; pictures and logos of the schools children will be attending.
- Reflective and going home books for parents to take home.
- Pictures of the classrooms children will be moving into to support familiarisation.
- Letters and sounds group times, story time and numeracy activities.
- Talking to the children about school routines.
- Mark making activities and looking at letters in the child’s name, fine motor activities getting fingers ready for writing for example: Dough Disco and Finger Gym.
- Literacy rich environments, reading areas and music sessions.
- Activities to support self-care skills for example putting their own coat on, toileting, handwashing, being independent at snack time, putting shoes on and taking them off.
Family hubs also liaise with schools/other professionals and invite teachers into the settings to observe children, with extended visits if required for children with Special Educational Needs (SEN) with a key person at the new school. Transition reports are also compiled for children. These are detailed developmental records which show where each child is in the prime and specific areas of learning.
Parenting sessions
Family hubs outreach deliver parenting sessions on toileting to the wider community. Potty Parties are held once a term to support children to be independent in toileting by providing information for parents as well as resources such as a potty, stickers and sticker charts. This support is also delivered in Private, Voluntary and Independent (PVI) settings where requested. A number of family hubs also support parents by offering dummy exchanges to help children to lose their dummies to promote speech and language and develop confidence and self-esteem.
Family hubs also host and deliver a number of different parenting programmes including; Sleep Success from two years old, Solihull from pre-birth upwards and Webster Stratton from three years upwards.
Early help interventions
Early Help interventions are delivered where family hub workers can complete home visits and signpost parents to groups and additional services. Family Support Workers can provide more intensive support with a group of professionals around them. This can involve work around boundaries and routines which in turn can help parents to prepare their child for school.
Opportunities for improvement or future development
- Strengthen the integrated review at two to two and a half years of age to include health, parent and early years setting.
- Potential to develop a School Readiness strategy.
- Develop more robust structures to support transitions to include all relevant professionals.
- Develop better information sharing, if consent given eg safeguarding information, any Early Help in place.
- Provide more support to PVI childcare provisions regarding skill and knowledge when assessing children’s developmental stages / transitions.
- Potential to work with primary care to ensure that children who aren’t in a setting are identified as ready for school.
- More work with schools to prioritise transitions with feeder settings, especially for children with SEN.
- Potential for a summer campaign over the six week holidays, for example: School Readiness Roadshow across communities to reach all children in the borough.
- Develop more ‘school readiness’ information for parents and other professionals ie what school readiness means and what their child should be able to do by the time they attend school.
Resources and supporting documents
Sleep
Why this is important
Sleep is an essential component of health and its timing, duration and quality are critical determinants of health. Sleep may play an important role in metabolic regulation, emotion regulation, performance, memory consolidation, brain recuperation processes, and learning. Due to the importance of these functions, sleep should be viewed as being as critical to health as diet and physical activity.
Insufficient sleep has major health consequences in adults, adolescents, and young children. Strong evidence exists that among adults insufficient sleep has a significant effect on numerous health conditions, including chronic disease development and incidence. Evidence also shows that children who experience short sleep duration are more likely to become obese than those who do not.
Insufficient sleep, unlike other health risk factors such as smoking, excessive alcohol consumption, obesity, and physical inactivity, has historically received much less attention in the public health and clinical settings. Insufficient sleep is an important public health risk factor that would benefit from further investigation.
The Royal Society for Public Health (RSPH) has warned that the UK public is under-sleeping by an average of almost an hour every night, which amounts to losing an entire night’s sleep over the course of a week.
RSPH polling has also shown that the public feel getting enough sleep is the second most important activity for optimising their health and wellbeing, ahead of health behaviours such as eating five fruit and vegetables a day, undertaking enough physical activity, and sticking to recommended alcohol guidelines. Indeed, sleep was ranked second only behind not smoking.
Insufficient sleep is costly for employers and society; not only does it lead to higher levels of absenteeism, but also increases presenteeism. A recent RAND Europe report investigated the link between insufficient sleep and workplace productivity, quantifying the economic costs. Insufficient sleep was found to cost the UK economy approximately £38 billion per year.
What we're doing and the assets or services we have
One of the key themes highlighted in the last Director of Public Health Annual Report, ‘A Day in the Life Of’, was sleep. This was due to the significant number of Barnsley residents revealing their feelings of tiredness during the day and how lack of sleep was affecting their day to day lives. As a result of this response, the report made a number of recommendations to raise the awareness of the importance of sleep.
Similarly, a recent Workplace Health Needs Assessment (2018) for businesses in Barnsley included a number of questions for employees in relation to sleep. The findings suggest a high proportion of employees who completed the workplace health survey have problems associated with their sleep and would like information or help to access sleep promotion activities at work.
With regard to guidance and support networks available in Barnsley, the focus is predominantly on young children and parents. Many parents can seek advice from health care professionals about sleeping and safety, particularly if they have concerns. Health visitors, midwives and general practice nurses are well placed to provide advice. The healthy child programme includes sleep guidance as part of the ‘pregnancy and first five years of life’. Discussions with parents about safe sleeping are part of maternity care, both antenatal and post-natal, as is support offered by health visitors. South West Yorkshire Partnership (Mental Health Access Team) offer a sleep workshop for adults experiencing issues with sleep.
Children with ongoing sleep difficulties would get referred to Sheffield’s Children Hospital as Barnsley does not commission a sleep service.
In order to improve better health in Barnsley, a more proactive approach is required to promote good sleep hygiene and minimise the impact of sleep loss for Barnsley residents. The multi-dimensional nature of sleep and the wide-reaching implications it has would require addressing all of these issues across a number of organisations.
However, there are measures that the council’s Public Health Service has taken to have an impact at a population level. The main focus of this has been to raise awareness among the general public, local businesses or organisations and managers and Barnsley Council staff.
In order to raise awareness among the general public, the first round of social media campaigns started in October 2018, predominantly featuring in the week leading up the change from British Summer Time to Greenwich Mean Time.
The messages during this campaign included:
- introducing a ‘slumber number’ as guideline hours of sleep each day, to provide guidance for the public on roughly how much sleep they should be aiming to have
- Sleep hygiene infographics (social media), to share sleep hygiene habits and practices, which describe the ideal conditions for a good quality sleep eg avoiding caffeine or eating a heavy meal at night etc.
Sleep hygiene messages used in the October campaign have been used in addition to other related messages on national sleep days throughout 2019:
• World Sleep Day (15 March 2019)
• Stop Snoring Week (22 to 26 April 2019)
• National Sleep Awareness Week (10 to 16 March 2019)
• National Sleep-In Day (30 October 2018)
• Clock change days (March and October 2019)
The general public, local businesses, organisations, managers and employees have been supported by providing them with a Barnsley Sleep Toolkit. Barnsley Council Public Health has produced a ‘Sleep and Recovery Toolkit’, which offers insight and advice on sleep loss. This tool kit has been adapted from a Public Health England document and shortened to make an easy read and follow document. The toolkit provides practical information and guidance on how businesses and managers can create an environment where employees understand the importance of sleep and recovery. The toolkit also gives valuable advice and sleep hygiene tips to employees and the general public and assists them to make healthier choices at work and at home.
Opportunities for improvement or future development
To work in educational settings promoting a local public health sleep campaign
Schools and colleges can have a positive impact by giving key messages on sleep hygiene and supporting students who may have issues. This would be in the institutions interest from a health and educational perspective.
Sleep to be covered in secondary school curriculum
Sleep education is included as part of personal health social and economic education within the curriculum to provide adolescents with knowledge as to the importance of sleep for health and wellbeing. To ensure schools have access to resources and lesson plans based on the available evidence.
Sleep hygiene in colleges
There is currently lack of understanding of how poor sleep is affecting students’ health, engagement and attainment in colleges. It is recommended that we work with Barnsley’s colleges to understand if this is an issue, and if so, work collaboratively on evidence based sleep hygiene interventions.
Resources and supporting documents
- NHS Choices - information on better sleep and how to get it
- HSE – Stress Management Standards
- Mental Health Foundation – how to sleep better guide
- Alcohol advice
- Smoking cessation
- Healthy eating
- Lullaby Trust
- Sleep workshops - South West Yorkshire Partnership (Mental Health Access Team)
Smoking
Why this is important
Smoking prevalence in Barnsley is reducing, but at 18.3% Barnsley still has one of the highest rates in the country.
Half of all smokers will die as a result of their addiction. It is the leading cause of preventable disease and death in England and has been identified as the single biggest cause of inequality in death rates between deprived and affluent areas. Smoking causes and exacerbates long term health conditions. Smoking is the biggest cause of cancer in the UK, being linked to 16 different types of cancer and is responsible for 7 out of 10 cases of lung cancer.
Not only is there a substantial health impact to the population, smoking costs the economy and health system significantly. In Barnsley alone, it is estimated that smoking cost the local economy a total of £63.5 million in 2018, which includes costs such as those associated with lost productivity, social care and smoking related house fires. Smoking costs the NHS in Barnsley approximately £11.7 million each year (ASH 2018).
Our vision is to create a smokefree generation in Barnsley where smoking prevalence is less than 5% and children and young people can grow up in a place free from tobacco, where smoking is unusual.
The Barnsley picture and how we compare
- Around 1 in 5 adults in Barnsley are smokers (18.3%), according to the national annual population survey (2019). This is significantly higher than the England rate of 13.9%.
- Out of 16 comparator authorities, Barnsley has the second highest rate, although it is not significantly higher than the rates in the other South Yorkshire authorities.
- Smoking prevalence in Barnsley has fallen in recent years (from 24.4% in 2012).
- Approximately 19% of deaths (in those aged 35 and over) in Barnsley are due to smoking.
- In 2018/19, there were almost 4,000 hospital admissions of Barnsley residents for diseases that were totally or partly due to smoking.
- There are large variations in smoking prevalence, with rates in Barnsley GP practices ranging from 8% in Penistone to 35% in the Central area of Barnsley.
- Smoking prevalence varies between different occupational groups. In Barnsley, in 2019, 30.2% of adults in routine and manual occupations were smokers..
- The proportion of smokers in Barnsley who successfully quit at 4 weeks (CO validated) (2,110 per 100,000 smokers aged 16+) is significantly better than the national rate of 1,113 per 100,000. Barnsley’s rate of 2,110 represents 775 smokers who successfully quit at 4 weeks in 2019/20.
- 14.2% of mothers in Barnsley smoke during pregnancy; significantly higher than the national rate of 9.6%, although there has been a downward trend since 2013/14 when the rate was 23.0%.
What we're doing and the assets or services we have
Stop smoking service
A local free stop smoking service is available to all smokers who live or work in Barnsley at a variety of locations across the borough. The service provides a range of free nicotine replacement therapy and expert behavioural support, either face to face, over the phone or online.
Smoking in pregnancy
All pregnant smokers in Barnsley are seen by a trained Stop Smoking Specialist Midwife and given one to one support to help them quit in order to protect both mother and baby. This service is delivered by the maternity team at Barnsley Hospital making smoking support a routine part of antenatal care.
Make smoking invisible
A range of voluntary smoke free areas have been successfully rolled out across the borough, primarily to help make smoking invisible to children and young people in order to reduce the number of them taking up the habit. So far in our journey to make smoking invisible, after public consultation, we have implemented smoke free play parks, smoke free town centre zones (PALs Square) smoke free markets and smoke free primary schools. The next stages in the programme; dependent on public consultation; may include smoke free high streets (starting with Hoyland), smoke free town centre, Glassworks and Library @ the Lightbox, smoke free secondary schools and smoke free Barnsley College.
Tobacco Control Alliance
Barnsley’s Tobacco Control Alliance contributes to the improvement of the health, environmental and economic status of people living and working in the borough through coordinated, effective and sustained action against tobacco by organisations and individuals working in partnership. The Tobacco Control Alliance is well attended by key partners from across the borough The Alliance is Chaired by the Deputy Leader of the Council.
QUIT programme at Barnsley Hospital
QUIT is a supportive programme to help patients, staff and visitors to quit smoking. Patients who smoke will be identified, offered brief advice, nicotine replacement therapy and referred to the on-site stop smoking service. Barnsley Hospital is a fully smoke free site.
Tobacco enforcement
Barnsley Council has a full time officer dedicated to tobacco enforcement. The role includes ensuring shops are adhering to all the tobacco laws and smoke free legislation such as plain packaging, keeping cigarettes behind shutters, underage sales and also investigating illegal tobacco sales, including both illicit and counterfeit.
Opportunities for improvement or future development
Over the coming months we will be refreshing our Tobacco Control Strategy, and this will be done through consultation with wider partners and the Tobacco Control Alliance. A National Control Strategy is due to be published in May 2021 and any priorities in the refreshed local strategy will be aligned to National priorities to ensure we are working to the same goals as regional and national colleagues, however, considering local need.
- Expansion of make smoking invisible into other areas, dependent on public consultation, in order to help reduce the uptake of smoking.
- Focused work with colleges and secondary schools in Barnsley to support young people to quit smoking and help prevent the uptake of smoking in the first place.
- Working with the stop smoking service to provide innovative and creative ways to reach those most at risk and hardest to reach, ensuring an equitable service which targets those most in need.
We have achieved significant improvements in our smoking prevalence rates in recent years and we must continue to keep this momentum going by driving forward this agenda and keeping it a priority area for the health and social care system.
Resources and supporting documents
- Public Health England (PHE) - Tobacco control profile - the Local Tobacco Control Profiles for England provide data and information on tobacco use, tobacco related harm, and measures being taken to reduce this harm at a local level.
- Barnsley ward profiles
- Smoke free school launch at Laithes Primary School
- ASH Ready Reckoner Tool 2018
Under-18 conceptions
Why this is important
In line with the regional and national picture, under 18 conceptions have gradually reduced in Barnsley over recent years. The current rate is the second lowest since 1998 and represents a 54% reduction, Although the reduction is fantastic news, there are large inequalities within Barnsley with rates varying enormously between certain wards of the borough.
It is important to acknowledge that not all young families experience significant adversity or poor health and educational outcomes and young people can be fantastic parents. Some families require nothing more than universal service input however others may need additional support to reach their full potential. However, teenage pregnancy can be a cause and consequence of educational, health and social inequality for young people and their children.
Young people who become pregnant are significantly more likely to have:
- Faced more challenges and experienced deprivation
- Been looked after by the local authority
- Be from a family with history of teenage pregnancy
- Been out of education, employment and training
- Experience of living with a learning disability
- Lower employment rates by the age of 30
- Life long experience of poverty
There is a graded relationship between teenage pregnancy and adverse childhood experiences with the more Adverse Childhood Experiences (ACE) a child has experienced, the more likely they are to become teenage parents.
Babies born to teenage parents are more likely to be:
- Still born
- Suffer infant mortality
- Of a low birth weight
- Not breastfed
- Living in poverty
Young families are more likely to experience:
- Emotional health and wellbeing issues (including post-natal depression)
- Smoking throughout pregnancy and after pregnancy
- Substance misuse
- Repeat pregnancies
- Domestic abuse
- A child death or injury that leads to a serious case review
- Children being removed
National evidence suggests that work to raise aspiration of young people and keep them in education for as long as possible can be a preventative factor for teenage pregnancy. Relationships sex and health education and access to youth friendly contraceptive and sexual health services, are also effective in reducing under 18 conceptions.
The Barnsley picture and how we compare
-
Barnsley’s 2019 rate for under 18 conceptions is 27.7 per 1,000. This is significantly higher than the regional and national rates of 19.3 and 15.7 respectively. When compared to statistical neighbours, Barnsley’s rate is the third highest.
-
The rate of 27.7 represents 105 conceptions to under 18's during 2019, an increase from 99 in 2018, and the second lowest number since 1998.
-
Barnsley’s under 18 conception rate has reduced by more than half since 1998.
-
More than half (52.4%) of under 18 conceptions in Barnsley in 2019 led to abortion; similar to the national rate of 53.0%.
Data from:
What we're doing and the assets or services we have
Barnsley’s Teenage Pregnancy Partnership is a multi-agency partnership of professionals across the borough including; public health, sexual health services, maternity services, targeted youth support, family hubs, colleges and area council managers.
The group oversees the local teenage pregnancy strategy and works to an action plan that is based around national evidence and local priorities. This strategy and the overall sexual health strategy is due to be relaunched in the Autumn of 2020.
Particular strengths for the partnership over the past 12 months include:
- Young people being able to access support from the teenage pregnancy midwife up until the age of 21 and continuity of care from maternity services.
- A pathway between sexual health and maternity services that provides outreach to young people at antenatal and postnatal stage to arrange access to appropriate contraception and sexual health screening.
- Every secondary school in Barnsley engaging in the public health commissioned offer of relationships and sex education.
- A large number of pharmacies in the borough now offer free emergency contraception to young people under the age of 25.
Opportunities for improvement or future development
The focus of the teenage pregnancy partnership has now been widened to include not only prevention but support for young people who do become parents.
The recommissioning of integrated sexual health services in July 2020 has created an opportunity to expand the current RSE offer to schools. Work is underway to develop an online RSE offer to support schools with training and resources. The facility for young people who access the sexual health clinic to be provided with an opportunity to receive RSE input and support from the team will also be added.
Scoping work has begun to strengthen pathways between pharmacies and the integrated sexual health service with the eventual aim to support direct referrals from pharmacies into clinic.
We are also working on:
- An extended offer for young families from the 0-19 Public Health Nursing Service.
- Promoting links between Maternity and Early Help Services to break down barriers young people may have to accessing support.
- A piece of consultation work involving young families.
- Linking in with regional colleagues to set a local agenda for teenage pregnancy.
It is acknowledged that teenage pregnancy is a complex issue that does not have a silver bullet however it is hoped that work taking place in the borough now will benefit children and young people in the future.
Resources and supporting documents
- Teenage pregnancy and young parents: good progress, more to do is a useful briefing for councillors and includes local case studies illustrating effective practice on both prevention and support.
- Supporting young parents to fulfil their potential is a briefing for councillors which highlights the importance of dedicated, coordinated support for young parents to achieve health and education equity for them and their children. Local case studies illustrate different models of support arrangements.
- A framework for supporting teenage mothers and young fathers provides commissioners and service providers a tool kit to review support arrangements for young parents.
- Getting maternity services right for pregnant teenagers and young fathers is a guide for anyone working in maternity services who will come in to contact with young people.
Unintentional and deliberate injuries in children (aged 0 to 4)
Why this is important
Unintentional injuries are one of the main causes of premature death and illness for children in England. Every year in England, 60 children under the age of five die from injuries in and around the home, which is one in twelve of all deaths of children aged one to four. 450,000 visits to A&E departments and 40,000 emergency hospital admissions occur in England each year because of accidents at home among under-fives.
It is difficult to give a true cost of treating children's accidents as outpatients and inpatients but in the past, it has been estimated at more than £275 million a year.
It can cost as much as £250,000 to treat one severe bath water scald. This figure does not reflect the long-term costs of prolonged treatment and rehabilitation or the cost of pain suffering to the child. Nor does it reflect the lifetime disfigurement or disability and the financial loss to the patient and family for work hours lost caring for an injured child.
Most childhood accidents happen between late afternoon and early evening, in the summer, during school holidays and at weekends. Factors such as stress, death in the family, chronic illness, homelessness or moving home increase the likelihood of the child having an accident. Some happen when the usual routine is changed or when people are in a hurry. Distractions and inadequate supervision are often the cause of accidents. Additionally, poor housing and overcrowded conditions lead to increased numbers of accidents.
The link between childhood injury and social deprivation is strong with children from the most disadvantaged families being far more likely to be killed or seriously injured due to accidents. Efforts to prevent childhood injury and accidents are most effective using a system wide approach with timely effective support which engages parents with early intervention evidence-based approaches.
The Barnsley picture and how we compare
- Barnsley’s 2020/21 rate of 125.7 per 10,000 for hospital admissions caused by unintentional and deliberate injuries in children (aged 0-4 years) is similar to the national rate of 108.7 per 10,000.
- Out of 16 comparator authorities, Barnsley’s rate is the seventh highest.
- The 2020/21 rate of 125.7 is the second highest since 2010/11, having fallen over recent years.
Data from:
Figure 1: The main causes of emergency hospital admissions for under-fives following unintentional injuries in and around the home in 2014/15-2016/17 (rate per 100,000 resident population of children aged 0 to 4 years)
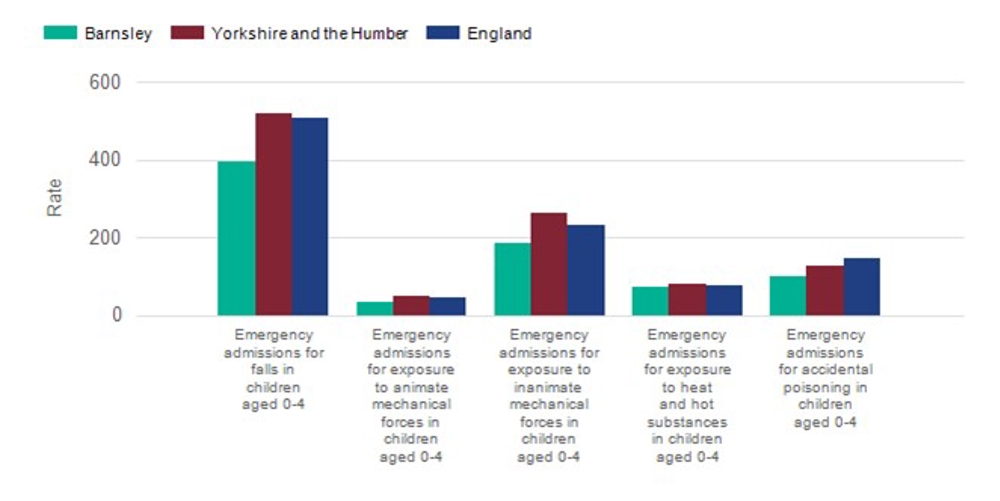
What we're doing and the assets or services we have
Barnsley takes a robust local system wide approach in the prevention and early intervention of childhood injuries in children aged 0-4 years, firmly locating the family at the centre of their work. This includes active engagement and collaboration across a range of agencies including 0-19 public health nursing service, children and family social care services, family hubs services, early help teams, early years settings and voluntary organisations.
This year, two areas of multi-agency service improvement have been established, both of which indicate a high level of commitment and collaboration in children and family services across Barnsley:
- A multi-agency sudden unexpected death in infancy (SUDI) task and Finish group was established in 2021. The group has developed guidelines and a training strategy for all agencies on a range of activities to support parents and carers to adopt safe sleeping practices for their infants.
- A multi-agency programme of work to support parents cope with their infant crying (ICON) has been delivered in 2021.
Amongst all services, social media has proven to become a well-used means to support universal child safety and accident prevention communications. This includes all year round, as well as seasonal timely messages, on safety and accident prevention on issues such as safe infant sleep-in hot weather or raising awareness of safety needs at bonfire night to prevent burns, hazards of fire, candles etc. Family hubs, BMC communications team, Public health nursing service all proactively post on their Facebook pages.
A range of children’s services use evidence based resources from the Child Accident Prevention Trust www.capt.org.uk and these are displayed in family hubs and leaflets can be provided to families where they are needed. CAPT resources are also used during child safety week to deliver local activities and events and promote safety messages in a fun and engaging way. Social media campaigns are also run during child safety week and throughout the year from family hub area pages and Virtual Family Hub Facebook pages.
Every parent in Barnsley is provided a Personal Child Health Record (PCHR) red book for their child at birth and this contains clear information on a wide range of safety issues and accident prevention.
Barnsley Public Health Nursing Service is a core universal service provided for children and young people aged 0-19 years. The service prioritises the health, wellbeing and safety needs of children and young people supporting parents to ensure that their children get the Best Start in Life.
Effective prevention and early intervention approaches ensure a targeted support offer for those families identified as living in more challenging circumstances.
The public health nursing team support parenting in early life stages, undertake health and development reviews at key stages of a child’s life as mandated through the Healthy Child Programme.
During the COVID-19 lockdown periods the public health nursing service took a proactive stance and delivered a blended programme of support to families, which included some essential face to face home visiting as well as the use of digital technology for none face to face contact. The service continued to provide parents with age-appropriate evidence based information and a range of activities to reduce childhood injuries including home safety assessments, providing information on preventing accidents, accessing safety equipment for families with additional needs and supporting effective use of safety equipment.
Key injury prevention areas covered include:
- Prevention of sudden unexpected death in infancy (SUDI) by working with parents and carers to undertake safe sleep risk assessments and develop safe sleep plans for their infants.
- Promotion of safe infant feeding - eg in relation to milk temperature
- Assessment of environmental factors, raising awareness of accident prevention in the home
- ICON coping with crying messages. Key touchpoints for health visitors following birth supporting prevention of abusive head trauma. Our SystemOne team has also set up a text message function to the new parent when the baby reaches 3 weeks with a message form the health visitor and online link to the ICON resources.
The public health nursing service is also a safe and well referral partner with South Yorkshire Fire and Rescue. The Safe & Well Referral Partnership Scheme aims to improve how the fire service and local organisations work together to effectively identify and reduce hazards for people most at risk. This enables SYFR and the PHN service to work together to keep our communities safer by SYFR carrying out Home Safety Checks or Safe & Well Checks for those most in need. Training has been rolled out within the service and staff have been set up with access to the SWFR referral portal. Practitioners in the service actively seek out charitable organisation to support vulnerable and disadvantaged families with home safety such as the Trussell Trust and Family Fund.
The public health nursing service receive discharge letters for all children attending an accident and emergency department, regardless of reason for attendance. This enables the service to identify and provide additional support to the parents whose child was injured, to liaise with other services working with the family and refer a family for additional support if required.
Family hubs provide a range of programmes for expectant or new parents Sleep tight across the borough from every family hub:
- Call the Push – CPR for parents, all outreach staff are trained to deliver
- All centres are part of Safeguarding Week this year offering first aid training to all our parents with a first aid box on completion.
- Throughout the year family hubs offer advice on road safety, car seat safety alcohol and drug awareness, mental wellbeing, toy safety.
- Through our parenting courses Solihull on line, Webster Stratton etc we have a golden thread of supervision of children.
Road safety activity across South Yorkshire is currently centred around the 3 E’s – education, enforcement and engineering. The majority of activity aimed at safeguarding 0 – 4 year olds falls into the education category – although notwithstanding that, enforcement and engineering activity is intended to increase safety for all road users.
Specific activity aimed at 0–4 years
SY Safer Roads Partnership (SYSRP) offer:
- Advice for parents around child car seats.
- Road safety packs for nurseries offering activities and stories (Smart Start); two stories aimed at nursery level teddy takes a tumble (seatbelt) and teddy takes a walk.
- Street feet sessions are offered by PCSOs using mini street scene and dressing up clothes.
Interventions in car safety for 0-4 year olds
- Sessions for parents in early years settings
- Specific car seat clinics
- Advice and information at events
- Encourage early years settings to use Smart Start resources around in car safety.
Data
- 6 out of 181 casualties in 2020 were known to be age 0–4. Taken from Department of Transport, there’s a full data tool available, which can be used to compare with other LAs.
South Yorkshire population/casualty rates
| Age | Car pass | Ped | PC | P2W | PSV pass |
| 0 to 4 | 0.54 | 0.31 | N/A | N/A | 0.14 |
| 5 to 10 | 0.89 | 0.86 | 0.27 | N/A | 0.05 |
| 11 to 16 | 0.89 | 1.58 | 0.50 | 0.31 | 0.16 |
Opportunities for improvement or future development
There is an opportunity to shape work locally National Institute for Health and Care Excellence (NICE) guidance PH29 and PH30 (2010), alongside PHE’s “Preventing unintentional injuries guide”, offer a framework for shaping the work locally particularly for vulnerable families.
The health visitor delivery model has been revised for 2021 to provide a service that is universal in approach and personalised in response, providing the public health nursing service with a framework to support effective prevention and early intervention in this area of work.
The cross party 1001 critical days supports early intervention to address the health and social inequalities which are more prevalent among 0-4 year olds who experience injury.
Better births: transforming maternity care sets out the need to enhance collaboration and communication between midwifery and public health nursing services and provides a framework for the early identification and intervention for parents with increased support needs.
Health protection
This section includes:
- childhood vaccination statistics
- HIV (late diagnosis)
- seasonal flu vaccinations
Childhood vaccination statistics
The Barnsley picture and how we compare
Read our childhood vaccination coverage statistics.
HIV (late diagnosis)
Why this is important
Late diagnosis of HIV leads to increased morbidity and the potential of life threatening illness. Hospitalisation and ill health place a significant challenge both to the individual and often their wider family (especially when the person affected has dependants).
People who are diagnosed at a later stage will have been infectious for a length of time before diagnosis meaning that there is a significant risk that HIV could have been transmitted to sexual partners if safer sex practices were not followed during that that period.
A person who is on a successful treatment regime resulting in undetectable levels of HIV in the body is no longer considered to be an infection risk to others during sexual activity.
It is also important to enable access to PrEP (Pre-Exposure Prophylaxis) which is now available to those people most at risk of HIV (only those who do not have a pre-existing HIV diagnosis). This will prevent them from getting HIV from unprotected sex or injection drug use. When taken as prescribed, PrEP is highly effective for preventing and reducing the transmission of HIV.
The Barnsley picture and how we compare
- Of those diagnosed with HIV in Barnsley (aged 15 years or more) in 2018-2020, over half (53.3%) were classified as being diagnosed at a late stage. This is higher than regional and national rates of 47.7% and 42.4%.
- When compared to statistical neighbours, Barnsley’s HIV late diagnosis rate is the seventh highest.
- The rate of 53.5% represents approximately three people per year in Barnsley who were diagnosed with HIV at a late stage.
- Barnsley’s late diagnosis HIV rates have fluctuated in recent years, with the highest being 74.4% in 2010-2012 and the lowest in 2014-2016 (39.2%).
What we're doing and the assets or services we have
-
We have commissioned an open access integrated sexual health service to provide free HIV testing. An integrated sexual health service means that almost everything relating to contraception and sexually transmitted infections (STI) needs is available in one place, including complex STI treatments and complex contraception problems.
Specifically in relation to HIV this means:
- Pre Exposure Prophylaxis (PrEP) is available to those most at risk of contracting HIV.(An antiretroviral medicine which, taken once a day, stops the transmission of HIV during unprotected sex) through our Integrated Sexual Health Service.
- Online STI and HIV testing is available to all Barnsley residents
- Co-ordinate notifications for STIs and HIV to partners.
- Risk assess cases and provide post-exposure prophylaxis (PEP) after sexual exposure to HIV. PEP involves taking antiretroviral (ARV) medicines very soon after a possible exposure to HIV to prevent becoming infected. Providing sexual health education to patients about HIV. Providing insight sessions at BEST meetings and training to other professionals.
- Ensure that our Sexual Health service makes good links with primary care.
- Take opportunities to engage with national HIV campaign opportunities (eg HIV testing week)
- Ensure that our sexual health services report and progress in relation to ensuring there is good access for those most at risk.
- Receive HIV testing data and review at least quarterly.
- Ensure that we have senior management scrutiny via the Health Protection Board.
Opportunities for improvement or future development
- A more tailored approach to advertising services targeted at those who are at higher risk of HIV and STIs will continue to be improved. Our online and outreach offer to those at higher risk will continue to improve.
- We will ensure that we continue to work collaboratively with the HIV treatment and care commissioner and provider.
- Partnership approaches to HIV testing within the community and improvement of referral pathways will continue to be developed and improved.
Resources and supporting documents
- Public Health Outcomes Framework - indicator D07
- Public Health England (Sexual and Reproductive Health Profiles)
Seasonal flu vaccinations
Why this is important
Flu vaccination is one of the most effective interventions we have to reduce pressure on the health and social care system this winter. We have seen the impact of COVID-19 on the NHS and social care, and during the winter we were faced with co-circulation of COVID-19 and flu. Those most at risk from flu are also most vulnerable to COVID-19.
For most healthy people, seasonal flu is an unpleasant but usually self-limiting (resolving itself without treatment) disease with recovery generally within a week.
However, some people are at particular risk of severe illness if they catch flu and are eligible for a flu vaccination.
Groups eligible for an NHS funded flu vaccination (2020/21) include:
- All children aged two to eleven (but not twelve years or older) on 31 August 2020
- People aged 65 years or over (including those becoming age 65 years by 31 March 2021)
- Those aged from six months to less than 65 years of age, in a clinical risk group
- All pregnant women
- Household contacts of those on the NHS Shielded Patient List, or of immunocompromised individuals
- People living in long-stay residential care homes or other long-stay care facilities
- Those who are in receipt of a carer’s allowance, or who are the main carer of an older or disabled person
- Front line health and social care staff
- People aged between 50-64 years
The Barnsley picture and how we compare
- Barnsley’s 2020/21 seasonal flu uptake rates for the over 65’s, under 65 years (at risk), pregnant women and two and three year olds are all slightly higher than the England rates.
- Barnsley also has good uptake rates in primary school age children, with more than two-thirds of children in Reception and Years one to three being vaccinated in 2020/21; again, higher than the rates nationally and regionally.
Data from
What we're doing and the assets or services we have
NHS England’s flu programme is a co-ordinated and evidence-based approach to planning for the demands of seasonal flu across England. The aim is to increase vaccine uptake rates, particularly among those who are most vulnerable to the effects of flu.
GP practices invite children aged two and three years, those aged from six months to 65 years with an underlying health condition, pregnant women and those aged over 65 years for a flu vaccination throughout the flu season (September – March).
Pharmacists, who are signed up to give the vaccine, offer flu vaccinations to those aged 18 and over with an underlying condition, to those aged over 65 years and to pregnant women throughout the flu season (September – March).
Barnsley Maternity services offer flu vaccination to pregnant women throughout the flu season (September – March).
A school-based flu vaccination programme is offered to all children in reception and school years one to seven.
The health care and social worker vaccination programme offers vaccinations for those employed in health care organisations, social care organisations, local authority organisations and private and community organisations across Barnsley.
Barnsley Council offers onsite vaccination clinics for its front-line health and social care workforce.
Opportunities for improvement or future development
Our key priorities and areas of focus include continuing to encourage uptake for those most at risk, 2- 3-year-olds and addressing vaccine inequalities. To continue to address vaccine inequalities through effective Public Health interventions, data analysis and targeted support focussing on people living in deprived communities, those with learning disabilities, people from black and minority ethnic backgrounds to take up the flu vaccine.
Wider determinants
This section includes:
- air pollution
- child poverty
- gambling
- road safety
- special educational needs and disabilities (SEND)
- social isolation
- young people not in education, employment or training (NEET)
Air pollution
Why this is important
The Government's Clean Air Strategy published in 2019 states that 'air pollution is the top environmental risk to human health in the UK, and the fourth greatest threat to public health after cancer, heart disease and obesity', and causes more harm than passive smoking. Fine particulate matter is an airborne pollutant contributing significantly to this environmental risk. It is defined as particulate matter less than 2.5 microns in diameter, and is referred to as PM2.5.
The strategy further states that:
'Conditions caused or exacerbated by air pollution include asthma, chronic bronchitis, chronic heart disease (CHD), and strokes. These conditions significantly reduce quality of life. They also mean that people are less able to work and need more medical care, resulting in higher social costs and burdens to the National Health Service.
'Poor air quality can affect health at all stages of life. Those most affected are the young and old. In the womb, maternal exposure to air pollution can result in low birth weight, premature birth, and stillbirth or organ damage. In children there is evidence of reduced lung capacity, while impacts in adulthood can include diabetes, heart disease and stroke. In old age, a life-time of exposure to air pollution can result in reduced life-expectancy and reduced wellbeing at end of life. There is also emerging evidence for a link between air pollution and an acceleration of the decline in cognitive function.'
The Barnsley picture and how we compare
- In 2019, it was estimated that 4.8% of all deaths in Barnsley in those aged 30+ were attributable to fine particulate air pollution; lower than the England rate of 5.1%.
- This also compares to the average in the Yorkshire and Humber area of 4.8%.
- Rates have declined since 2013.
What we're doing and the assets or services we have
Barnsley Council’s Regulatory Services are responsible for dealing with fine particulate pollution and air pollution as a whole under the Local Air Quality Management (LAQM) regime. LAQM is a statutory duty under the Environment Act 1995.
Delivery of LAQM involves collaborative work with other local authorities, Highways England, the Environment Agency and other stakeholders. The work also includes assessing the impact of potential Clean Air Zones.
LAQM requires local authorities to undertake regular reviews and assessments of air quality in their areas to identify whether the health-based air quality objectives have been or will met by a specified date. In situations where these objectives will not be achieved, local authorities must declare the location as an Air Quality Management Area (AQMA), and prepare an action plan which identifies appropriate measures that will be introduced to achieve the objectives.
Barnsley has six AQMAs that have been declared due to breaches of annual mean concentrations of the polluting gas nitrogen dioxide which is strongly associated with traffic emissions. Barnsley’s Air Quality Action Plan (AQAP), whilst primarily dealing with reducing nitrogen dioxide gas concentrations, also tackles PM2.5 concentrations, (PM2.5 are tiny particles in the air that reduce visibility and cause the air to appear hazy when levels are high) as the actions to reduce concentrations of nitrogen dioxide and PM2.5 are broadly similar.
A steering group, chaired by the Director of Public Health, oversees the implementation of the AQAP. The implementation of the wide-ranging AQAP actions is the responsibility of internal Council and external stakeholders and requires significant officer resource.
Regulatory Services own and operate two continuous air quality monitoring stations in the borough, and undertake air pollution sampling at 64 other sites. It has contracts with specialist laboratories and equipment suppliers to ensure the accuracy of air quality monitoring. Regulatory Services have also joint ownership (along with the other South Yorkshire Councils) of a sophisticated emissions database and air pollution modelling system.
Central Government have contracted Regulatory Services to manage two Government owned air quality monitoring stations, one in Barnsley and one on the outskirts of the borough border.
Opportunities for improvement or future development
Following the incorporation of Regulatory Services into Public Health, opportunities for joint working to improve local air quality and local health have been recognised. Common synergies include promotion of the active travel agenda, anti-idling, eco driver training and raising awareness of air quality within schools. Some of this work is beyond the statutory remit that Regulatory Services are required to undertake, but will be of benefit to local people. As a result, Public Health have identified resources to progress and develop this joint agenda.
Subsequent to the publication of the Clean Air Strategy in 2019, the Environment Bill has now been laid before Parliament, with the Bill currently expected to become law sometime later this year. The key air quality proposals include consideration of a new, more stringent air quality standard for PM2.5, possibly based on the World Health Organisation target for PM2.5, although the new standard is not expected to become law until later in 2022. Regulatory Services will assess the implications of the proposed standard when further information is made available, along with proposed changes to the Smoke Control Areas legislation to manage domestic burning (a source of PM2.5).
Resources and supporting documents
Child poverty
Why this is important
The Marmot Review (2010) suggests there is evidence that childhood poverty leads to premature mortality and poor health outcomes for adults. Reducing the numbers of children who experience poverty should improve these adult health outcomes and increase healthy life expectancy.
There is also a wide variety of evidence to show that children who live in poverty are exposed to a range of risks that can have a serious impact on their mental health.
"A New Approach to Child Poverty: Tackling the Causes of Disadvantage and Transforming Families' Lives" sets out the Government's approach to tackling poverty for this Parliament and up to 2020. This strategy meets the requirements set out in the Child Poverty Act 2010, focuses on improving the life chances of the most disadvantaged children, and sits alongside the Government’s broader strategy to improve social mobility.
The Barnsley picture and how we compare
The Children in low-income families indicator illustrates the proportion of children living in families in receipt of out-of-work benefits or tax credits, where their reported income is less than 60% of UK median income.
Although the latest data (2016) is not as up to date as we would prefer, it shows that for children in Barnsley:
Aged under 20
- More than two out of five (21.6%) live in poverty; significantly higher than the national rate of 17.0%.
- Compared to similar local authorities, Barnsley’s rate is the fourth highest.
- The rate has fluctuated since 2006, and the 2016 rate is the second lowest during the period.
Aged under 16
- More than two out of five (21.9%) live in poverty; significantly higher than the national rate of 17.0%.
- Compared to similar local authorities, Barnsley’s rate is the third highest.
- The rate has fluctuated since 2006, and the 2016 rate is the second lowest during the period.
It is worth bearing in mind that some eligible families do not claim their benefit entitlement, whilst others may be living in income deprivation but may not be entitled to claim.
Another measure of poverty in children under 16 years is also available: the Income Deprivation Affecting Children Index (IDACI) from the 2015 Indices of Multiple Deprivation (IMD) 2015*. This shows that:
- Barnsley’s rate of 24.9% is significantly higher than the England rate of 19.9%.
- Compared to similar local authorities, Barnsley’s rate is the fifth highest.
- Within Barnsley, there are large differences, with rates ranging from 41.2% in Dearne North to 5.5% in Penistone East.
* The IMD 2019 was published on 26 September 2019 – further analysis at Barnsley and ward level will follow.
Data from:
Resources and supporting documentation
- A New Approach to Child Poverty: Tackling the Causes of Disadvantage and Transforming Families
- Fair Society Healthy Lives (The Marmot Review)
- The Children’s Society, Effects of child poverty
Gambling
Why this is important
Gambling is increasingly recognised as a public health issue, contributing to ongoing health inequalities, the experience of physical and mental health problems (including suicidality) and poor wellbeing. Gambling-related harms are often not recognised and require greater attention. The legislative framework for gambling recognises it as a legitimate leisure activity that many people enjoy. It generates income, employment and tax revenue. Set against this, it also generates significant dis-benefits such as working days lost through disordered gambling, or the cost of treatment for ill-health caused by stress related to gambling debt. Less easily measured are potentially very significant impacts such as the negative effects of some gambling on family relationships, and the psychological and social development of children.
Gambling has been described as being, like alcohol, a legal activity on a continuum of harm. It has been suggested that there are a large number of people experiencing small amounts of harm from gambling, and a small number of people that experience high levels of harm. A report by Citizen’s Advice states 'The majority of people taking part in gambling do so responsibly and without risk. But for hundreds of thousands of people who are defined as problem gamblers, the impact can be devastating, including mental health problems, debt and relationship breakdown'. Participation in gambling can range from social and recreational gambling to disordered, compulsive, pathological, or problem gambling. The continuum ranges from 'non-problem' to 'at risk' and 'problem gambling' (The Cochrane Collaboration 2012, p6). It is estimated that gambling-related harm affects six to ten individuals close to the problem gambler.
Problem gambling or gambling-related harms can affect many different areas of an individual’s life, but the impacts are also wider than the individual concerned, affecting social networks and society.
The Barnsley picture and how we compare
A report on gambling behaviour in England and Scotland describes the problem of quantifying problem gambling at a population level: 'there is no gold standard or commonly accepted way to measure problem gambling in population based surveys' (Seabury and Wardle, 2014).
This report offers two different modelled estimates, a national Gambling Commission (2015) estimate applied to Barnsley (0.8% prevalence) and Leeds Beckett University’s (Kenyon et al. 2016) Northern cities estimate (1.8%).
View the trend and comparator data charts for gambling.
It should be noted that Leeds is not a statistical neighbour of Barnsley, therefore direct comparisons to population estimates cannot be made. The demographics (race, religions, deprivation, age etc) of Leeds and the people interviewed will be different to those in Barnsley. Therefore, direct comparisons should not be made.
What we're doing and the assets or services we have
BMBC Public Health are embarking upon examining problem gambling in Barnsley and are in the process of establishing a task and finish group to verse this work.
The current treatment system for problem gambling for adults is commissioned through Gambleaware & Gamcare. There is no NHS or Local Authority funded specialist treatment for problem gambling in Barnsley. However, the first NHS gambling clinic and support services, outside of London, opened in Leeds on the 18 September 2019. This specialist service will cover the North East, North West, Yorkshire and Humber and the Midlands area.
The service will link in and collaborate with services already set up in the UK such as the national gambling helpline and local GamCare services. There will be a strong referral pathway between the Northern Gambling Clinic and GamCare services, with patients able to move in both directions, and in some cases care would be shared for a period.
In addition to the national helpline, the service has its own direct referral system, in addition to the usual routes of self-referral, GP referral, professional referral etc. Links with mental health services, the criminal justice system, the homeless community, and black and minority ethnic (BME) community would be made, in partnership with GamCare where appropriate. The service also has its own website with contact details, and resources for service users and their families.
Specialist support for gambling at Tier 1 (universal services) is provided through the GamCare Helpline/ net line including support, advice and signposting. The only locally provided specialist service in Barnsley is Krysallis in partnership with GamCare who provide (Tier 2 and Tier 3) talking treatments utilising an evidence based model of care of extended brief interventions and psychosocial sessions. Face to face, phone and online support is available and Krysallis also offer aftercare sessions.
Opportunities for improvement or future development
Barnsley Council Public Health will take appropriate steps to comply with the suggestions made within the ‘tackling gambling related harm – a whole council approach’ guidance report and address the issue of harmful / problem gambling under the Health and Wellbeing Board.
Harmful / problem gambling will be included within the following council strategies:
- Suicide prevention action plan
- Homeless strategy
- Domestic violence strategy
- Statement of licencing policy (for gambling)
- Anti-poverty action plan
- Alcohol strategy
Problem gambling is often seen alongside other dependences and mental health difficulties, therefore it is likely that many problem gamblers are already receiving support from services in Barnsley. Sheffield Council has completed an audit of all front line services in the community, including primary care, and this is something the council’s Public Health service will replicate. The purpose of the audit will be to establish a baseline of how many organisations in Barnsley are equipped to identify, treat or refer problem gamblers. The results of the audit will be used to identify any actions needed to increase the capacity of local organisations to identify and help address problem gambling.
If it is identified from any service audits that there is a training need for front line staff (including primary care) in Barnsley, training can be provided free by Calderdale Citizens Advice Bureau, and is in line with recommendations from the ‘tackling gambling related harm – a whole council approach’ guidance report.
Due to the high prevalence of young people experiencing issues with problem gambling nationally the council’s Public Health service will aim to include questions about gambling in to the health education and lifestyle survey 2019.
Using good examples from regional colleagues, mainly Leeds and their ‘Beat the Odds’ campaign, the council’s Public Health service will develop and roll out a local campaign around gambling related harms.
Resources and supporting documents
Road safety
Why this is important
The UK has a good record of reducing road casualties over the past 30 years, and was ranked third in Europe in 2017 for number of road deaths per million inhabitants. However, fatality reduction in the UK has plateaued since 2010, and in 2020, 1460 people were killed as a result of road incidents in Great Britain, and a further 23,529 people were seriously injured. Road traffic collisions are a major cause of deaths in children and young people in the UK, comprising higher proportions of accidental deaths as children get older.
Every death and serious injury on the road is a preventable tragedy. Road injury results in wide and long-term health consequences including physical disability, stress, cognitive or social impairment, lower educational attainment and lower employment prospects. The average medical and ambulance cost to the NHS are estimated to be approximately £14,000 for every serious road injury, although this excludes other costs related to long-term treatment, social care costs, social security costs and productivity losses. The total value of prevention of reported road injury accidents is estimated to be £12billion a year.
There are ongoing inequalities in injury rates across the UK. The highest rates of both hospital admissions and police-reported serious and fatal casualties result immediately after young people can start legally using cars and motorcycles. Males are at greater risk of being killed in traffic; more than three male children or young people die on the road for every female child or young person who dies. Children and young people who live in more deprived areas are at a much greater risk of road injury than children from the most affluent areas; more than one quarter of child pedestrian injuries across England occur in the most deprived wards.
Car occupants constitute the largest road user group and have the highest number of injuries and fatalities each year. However, pedestrians, cyclists and motorcyclists have a much higher casualty rate (casualties per mile travelled) and fatality rate (fatalities per mile travelled) and are considered to be vulnerable road users.
Data from
- GOV.UK: Road safety statement 2019: a lifetime of road safety
- DfT: Reported road casualties in Great Britain: main results 2018
- GOV.UK: Reported road casualties Great Britain, annual report: 2020
- GOV.UK: Major causes of death and how they have changed
- GOV.UK: Reducing unintentional injuries among children and young people
- DfT: Reported road casualties in Great Britain: 2017 annual report
The Barnsley picture and how we compare
- In 2020, Barnsley’s rate of people who were killed or seriously injured on roads (100.7 per billion vehicle miles) was similar to the England rate of 86.1.
- Out of 16 comparator authorities, Barnsley’s rate was the highest.
- In terms of numbers, the 2020 rate of 100.7 per billion vehicle miles equates to 114 people who were killed or seriously injured on roads in 2020.
- The 2020 rate is the second lowest since 2017.
- In 2014-16, the proportion of alcohol related road traffic accidents was 24.2 per 1000 accidents, which is similar to the England rate of 26.4 per 1000
Children and young people
- In 2017/19 the proportion of children under 16 who were killed or seriously injured on the roads (50.4 per 100,000) was significantly higher than the England rate of 18.0 per 100,000.
- Between 2015/16 and 2019/20, the proportion of emergency admissions of motorcycle riders aged 0-24 years involved in road accidents in Barnsley (14.5 per 100,000) was similar to the England rate of 11.4 per 100,000.
- The proportion of motorcyclists killed or seriously injured in road traffic accidents aged 15-24 (2015-19) in Barnsley was 22.6 per 100,000, similar to the England rate of 6 per 100,000.
- The proportion of car occupants killed or seriously injured in road traffic accidents aged 15-24 (2015-19) in Barnsley was 57.9 per 100,000, significantly higher than the England rate of 29.4 per 100,000.
- The proportion of emergency admissions for pedal cyclists aged 0-24 (2015/16-19/20) was 11.6 per 100,000 which is similar to the England rate of 12.9 per 100,000.
Data from
- Public Health Outcomes Framework (indicator B10)
- Public Health England Child and Maternal Health Profile
What we're doing and the assets or services we have
Within the Barnsley Council’s Corporate Plan 2021 – 2024, one of the stated aims is that people are safe and feel safe. Barnsley Council’s Transport Strategy 2014-2033 highlights their priority to promote safety, security and health in Barnsley. Barnsley Council is a member and funder of the South Yorkshire Safer Roads Partnership (SRP); a multi-agency, multi-functional partnership which includes the four local highway authorities in South Yorkshire (Barnsley, Doncaster, Rotherham and Sheffield), South Yorkshire Police (including South Yorkshire Safety Cameras), South Yorkshire Fire and Rescue, the Peak District National Park, South Yorkshire Passenger Transport Executive, Highways England and the University of Sheffield. The primary objectives of this partnership are to reduce the number of people killed and injured as a result of a road traffic collision and to make South Yorkshire roads safer.
The SRP provides a range of valuable road safety activity in Barnsley, and actively contribute to our local Road Safety working group. SRP provide data cleansing, validation, analysis and presentation, including an online dashboard of collision data in Barnsley. In addition the SRP run a number of road safety campaigns both on social media and through traditional advertising. They provide education in schools for year 6 – year 11 pupils, using a mixture of virtual and in person training, focussing on high-priority schools. In addition, training sessions are offered to businesses that have staff who drive for work purposes and Biker Down! first aid/first on scene training is offered to motorcycle riders. The SRP also provides quarterly casualty data analysis to support the prioritisation and development of interventions and provides communications support through the SRP website and social media channels and a campaigns calendar. The SRP attends events across South Yorkshire, targeting key audiences and utilising SRP assets such as the community engagement vehicle. The SRP also supports monitoring and evaluation through the use of the joint activity database which records schools delivery and RS Evaluate which collects, collates and analyses the data.
Barnsley Council has also established a local, safer roads working group which brings together key local stakeholders from both services within the Council, such as Engineering, Highways, Public Health and Communities along with key partners such as South Yorkshire Police and South Yorkshire Fire and Rescue. This group is responsible for overseeing the development of a local Road Safety strategy, and driving improvements in road safety locally.
In 2020, Barnsley Council’s Public Health Team published a ‘Road Injury Health Needs Assessment’ which analyses the extent of road injuries in Barnsley and provides a range of recommendations to improve safety on our roads. Implementing these recommendations is being led by the local safer roads working group.
Fatal incidents are all reported directly to the Council’s Transport Group and investigated. In addition, the Transport Group undertakes annual cluster site analysis to determine if road safety engineering measures are required.
Opportunities for improvement or future development
- Through the local Road Safety Working Group, Barnsley Council are beginning to develop a local Road Safety Strategy, which builds upon the recommendations contained within the recommendations contained within the 2020 Health Needs Assessment.
- Further analysis of the Barnsley casualty data is planned, to support prioritisation and development of interventions
- The use of publicity and local campaigns to deliver targeted road safety messages, including digital media is being considered – especially considering how this can complement the offer of the SRP.
- Continuing to implement the recommendation contained within the 2020 Road Injury Health Needs Assessment.
SEND
Key points
- The total number of children on the current SEND register in Barnsley is 4945, around 15% of all pupils. The most common primary diagnosis of SEND is moderate learning difficulty (MLD), followed by social, emotional and mental health (SEMH), speech, language and communication (SLCN) and autistic spectrum disorder (ASD).
- Barnsley has a different pattern of primary diagnosis compared to other areas in particular a higher proportion of pupils with MLD and lower proportion of pupils with specific learning difficulty (SLD).
- Those families living in the most deprived areas of Barnsley are disproportionately more likely to have a child with SEND. Tackling poverty and ensuring low income families are receiving the support they need is central to improving outcomes and reducing demand.
- Barnsley has a comparatively higher percentage of SEND pupils with an EHCP and lower percentage of SEND pupils with SEN support. In particular pupils with physical disability (PD), SLCN and SEMH are more likely to have an EHCP compared to national figures.
- Although a comparatively higher percentage of EHCPs happen in Barnsley, further work is required to identify if those living in the most deprived areas are able to access EHCPs as well as those in less deprived areas.
- Barnsley has a greater proportion of pupils with a SEMH primary need, especially in secondary school pupils. Data from early years assessment and development checks show fewer Barnsley children are achieving an expected level of development in Personal, Social and Emotional Development (PSED).
- Those in living in Barnsley with experience of SEND are more likely to experience fixed term exclusion than those without SEND. Work with education to identify the reasons for this and possible solutions is warranted to ensure equity of education.
- A high proportion of referrals to CAMHS referrals do not require assessment or intervention – indicating inappropriate referral mechanisms. Work is being done locally to strengthen pathways, embed early intervention (through partnership work with family hubs) and provide guidance potential referrers.
- Strategic and operational work in Barnsley is moving at a great pace to improve health, educational and social outcomes for families affected by SEND.
Background
Definition of population
Special Educational Needs
The Special Educational Needs and Disability (SEND) Code of Practice (part of the Children and Families Act, 2014) defines SEN as:
- A child or young person has SEN if they have a learning difficulty or disability which calls for special educational provision to be made for him or her.
- A child of compulsory school age or a young person has a learning difficulty or disability if he or she: Has a significantly greater difficulty in learning than the majority of others of the same age, or has a disability which prevents or hinders him or her from making use of facilities of a kind generally provided for others of the same age in mainstream schools or mainstream post-16 institutions.
- For children aged two or more, special educational provision is educational or training provision that is additional to or different from that made generally for other children or young people of the same age by mainstream schools, maintained nursery schools, mainstream post-16 institutions or by relevant early years providers. For a child under two years of age, special educational provision means educational provision of any kind.
The main categories of SEN include:
- Communicating and interacting
- Cognition and learning
- Social, emotional and mental health difficulties
- Sensory and / or physical needs.
Disability
The Equality Act (2010) defines a disability as:
“a physical or mental impairment that has a ‘substantial’ (completing a task takes much longer than is usually would and ‘long-term’ (12 months or more) negative effect on ability to do normal daily activities. Sensory impairments and long term conditions are included in this definition.
There is overlap with young people who experience SEN also having a disability however not all young people with a disability experience SEN. In educational settings if a child or young person requires special educational provision, they would fall under the SEN umbrella.
For the purposes of this content, SEND will be used to discuss the population, unless explicitly stated otherwise.
National picture
It is estimated that 8% of children nationally have a recognised disability. Of those with a disability social/behavioural was the most common type of disability (42%) followed by learning (36%). As of January 2019, 14.9% of school aged pupils have a special educational need. Of those, the most common presenting need was Speech Language and Communication (SLCN) (22% of all pupils with SEN), followed by Moderate Learning Difficulty (MLD) (20%) then Social, Emotional and Mental Health (SEMH) (17%). For those with education, health and care plans (EHCPs), the most common primary need is autism spectrum disorder (ASD). 29% of these pupils have this as their primary need.
A changing landscape
On 1 September 2014, the Children and Families Act came into effect and with it a number of changes to how local authorities support children and young people with SEND and their families, particularly around assessment, planning and involvement in their care. One of the biggest changes was the age range expanding to include children and young people from birth to age 25. Additionally, local authorities are required to provide children, young people and their families with information and advice as well as details about services they can access in the local area, known as the Local Offer. Read more on Barnsley's Local Offer.
Under the new guidance, children and young people (CYP) can be offered SEN support from an educational provider, such as their nursery or school, which should meet their needs. SEN Support is generally managed by education providers and works on the principles of; assess, plan, do and review. For those requiring a more intensive level of specialist help, local authorities will carry out an education, health and care assessment. The outcome of this assessment could be an EHCP, which brings health, education and social care needs into one legal document. Children and families should be involved in all stages of this process. Further information about SEN Support and EHCPs can be found in the SEND Code of Practice.
The number of pupils with a Special Educational Need has been increasing over recent years and the overall figure stands at 1,318,300 children (14.9% of total pupil population). Of those, 3.1% (271,200 pupils) have an EHCP and 1,047,200 require SEN support (11.9% of pupil population).
SEND and equity
Children and young people with SEND often face multiple barriers which can make it more challenging for them to reach their full potential. They are more likely to be grow up and continue to live in poverty, more likely to be excluded from school and less likely than other children to attain good educational outcomes. This impacts on employment prospects, life chances and health outcomes. Timely identification of those children and young people to provide quality support can help reduce the inequality of outcomes that they face.
SEND in Barnsley
Local context
Barnsley is home to an estimated 55,800 children and young people and this is set to rise to 57,600 in 2023, a steady increase of just below 1% per annum. Of those young people, 13.0% of primary aged children have SEND with the number being 13.4% for secondary age young people14. Due to the steady population increase, if the proportion of CYP with SEND remains the same, this will result in an increase in actual numbers, year on year.
Barnsley’s under 18 population is predominantly white British (95.2%) with only 5.8% from black and minority ethnic (BME) groups. 6% of primary school children and 4% of secondary school children in Barnsley do not have English as their first language.
Barnsley is the 39th most deprived local authority in England with nearly 22% of its lower super output areas (LSOAs) being amongst the 10% most deprived in England. In particular Barnsley is ranked amongst the lowest 20 local authorities for the domains of skills and training, employment and health and disability and is the 10th lowest for education, skills and training.
An estimated 18% of children in Barnsley (9,004) are growing up in poverty, which rises to 28% (14,182 children) when housing costs have been accounted for. In Barnsley, around 17% of all school children are eligible for free school meals, a proxy indicator for deprivation, but this rises to 40% of children who have an EHCP and 36% of those with SEND support.
40% of Barnsley’s secondary schools are rated good or outstanding by Ofsted. This is below the regional and national rates. 83% of Barnsley’s primary schools are rated good or outstanding by
Ofsted. This is higher than the regional average and in line with the national average. 98% of early years childcare settings are rated good or outstanding by Ofsted. This is above the regional and national averages.
3% of Barnsley’s 16-17 year olds are Not in Education Employment or Training (NEET). This is lower than the regional and national rates of 3.7% and 3.2% respectively.
The total number of children on the current SEND register in Barnsley is 4945, accounting for 14.7% of all pupils. This includes only those who have been identified and placed on the register and may be an underestimate of actual need. Around 75% of pupils have SEN support and 25% have an EHCP15. Girls represent a quarter of pupils with EHCP and around a third of pupils with SEN support15. The ratio of boys to girls receiving CAMHS support for ASD is approximately 2:1.
Whilst the overall proportion of pupils with SEND in Barnsley has remained similar since 2016 and is in line with England, following a national increase, the relative type of support pupils are receiving is different to other areas.
Barnsley has a comparatively higher percentage of SEND pupils with an EHCP, than our statistical neighbours, 4% compared to 3.3 (3.1% England) and this has increased since 2016. Furthermore in contrast to national and regional trends, the percentage of pupils with SEN support has decreased for both primary and secondary schools since 2016, and is now 10.7% overall. This is 2.6% lower than any of our statistical neighbours. These differences are true for both primary and secondary schools but are more marked for secondary schools.
The cause of these differences is not known, although it is generally recognised nationally that identification of SEND can be inconsistent, leading to both under-identification and over-identification. This is an area which would benefit from further in depth analysis looking at the effectiveness of SEN support provision, whether there is pupil movement from SEN support to EHCP, the processes and thresholds used in Barnsley and how these compare to elsewhere.
Types of need
The most prevalent formal diagnoses for pupils with SEND in Barnsley are MLD (1325), (SEMH) (1061) and (SLCN) (964). Whilst SEMH and SLCN are two of the three most common primary needs for both pupils with an EHCP and SEN-support, the most common primary need for EHCP pupils is ASD, and for SEN-support pupils it is MLD. Although this is a similar pattern to England in terms of most common primary diagnosis, Barnsley has a higher proportion of pupils with SEMH as a primary need than England or other similar areas, for both primary and secondary schools.
Percentage of pupils with an identified need by type of need, 2019/20 academic year
| SEN description | Barnsley | England | Statistical neighbours |
| Moderate learning difficulty | 24.8 | 18.9 | 22.1 |
| Social, emotional and mental health | 23.0 | 18.3 | 18.8 |
| Speech, language and communications needs | 19.3 | 21.9 | 19.2 |
| Autistic spectrum disorder | 12.5 | 11.8 | 11.0 |
| Specific learning difficulty | 8.0 | 12.2 | 12.8 |
| Other difficulty/disability | 2.5 | 4.2 | 3.2 |
| Physical disability | 3.0 | 2.9 | 3.2 |
| Severe learning difficulty | 1.4 | 2.6 | 2.9 |
| Hearing impairment | 1.8 | 1.8 | 1.8 |
| NSA/not recorded/blank | 0.0 | 0.0 | 0.0 |
| Visual impairment | 1.0 | 1.0 | 1.0 |
| Profound and multiple learning difficulty | 0.9 | 0.9 | 0.9 |
| Multi-sensory impairment | 0.2 | 0.3 | 0.3 |
| SEN support but no specialist assessment of need | 1.5 | 3.2 | 2.7 |
Data from: Department for Education. Statistics Special Educational needs, 2019.
There is also a far higher proportion of MLD than England and comparison areas in Barnsley overall but particularly in secondary schools, 35.6% compared to 22% for England and is the highest amongst statistical neighbours.
Barnsley also has a lower proportion of pupils with a primary need of specific LD compared to elsewhere, especially in secondary schools, 8.5% compared to 20.5% for statistical neighbours. These differences are maintained when four year data is combined.
In primary schools the predominate primary need are SLCN, MLD and SEMH. The percentage of SEMH is around three percentage higher than national and regional figures and the highest out of all statistical neighbours, whereas percentages for SLCD are lower. ASD is as a primary diagnosis is also a few percent higher than elsewhere.
In secondary schools the predominate need is MLD followed by SEMH. In Barnsley the proportion of SEMH in secondary school is nearly 5% higher than other areas and is the second highest amongst statistical neighbours. In specialist schools 21% of pupils with SEND have SEMH as their primary need and 25% have ASD.
When comparing the percentage of pupils with each primary diagnosis (SEND-support or EHCP) in Barnsley to England figures, there are some clear differences. A higher proportion of Barnsley pupils with physical disability, SLCN and SEMH are supported with an EHCP compared to England. This is also true for those with visual impairment and multi-sensory impairment but as the numbers of pupils is small for these primary needs, this may represent a less significant difference.
Differences by age
The percentage of new and current children with EHCPs who are under the age of 5 in Barnsley is lower than the national figures. Nationally around 23% of new EHCPs are provided to children under five compared to around 14% in Barnsley, which has decreased from around 19% in 2016. Numbers of pupils identified as having MLD requiring SEN support start to increase from year 1, peaking at year 5 whereas numbers with an EHCP are relatively small until year 8. This does not appear to be the case for other SEND needs. The reason for this is not known but it may reflect later identification of some of these pupils or a movement from SEND support to EHCP which combined with the earlier findings of low numbers of SLD and high numbers of MLD means this should be an area of further focus.
SEMH appears to peak at Y4, with a large increase in SEN support from N2 to Reception, with EHCP numbers also highest in Y4. It may be that some of these children could benefit from being supported earlier.
Local inequalities and SEND
There is a complex relationship between poverty and SEND. Children from low income families are more likely to be born with or develop SEND and those with SEND are more likely to experience poverty. The proportion of children with SEND who are living in poverty also increases with age. Access to high quality early years provision has a particularly positive impact on those children with SEND but also those growing up in poverty who are at higher risk of SEND.
Pupils with SEND are more likely to be eligible for free school meals (FSM), 28% compared to 13% of pupils without SEND. Those with EHCPs are also more likely to be eligible for FSM than those on SEN support, 33% compared to 27%. This difference is greater for those with a primary need of SEMH, where the percentage increases to 34% of pupils with SEN support and 43% of pupils with an EHCP eligible for FSMs. Further work to establish the links between SEMH, poverty and SEND is warranted.
There are several factors linked to poverty which increase the likelihood of SEND, for example smoking during pregnancy and low birth weight. Mothers who do not have any formal educational qualifications are over two times more likely to have children identified as having SEND than those with a degree. This highlights that more work needs to be done to improve health and social inequalities across our communities.
There are also other factors either in pregnancy or soon after birth that can lead to additional needs. This could be the maternal illness in pregnancy, problems at birth, genetic factors or early childhood illness. Sometimes the cause is unknown.
In Barnsley much of the identified SEND need is concentrated within the more deprived areas. Whilst need has gone up for the most common primary diagnoses between 2016-19 for all deprivation quintiles, this has shown a higher increase for those children living within the most deprived areas compared to those living in the least deprived areas, increasing by 1.3% in the most deprived compared to 0.5% in the least deprived. This shows that the inequality gap has increased.
The Dearne locality has a much greater proportion of children with SEND compared to Barnsley, particularly in secondary school, 21.8% compared to 12.9%. The three highest levels of SEND in primary school are found in St Helen’s, Dearne South and Stairfoot wards and the three highest for secondary school are Dearne North, Dearne South and St Helens. These are all areas which have a high proportion of LSOAs which are within the 10% most deprived in the country.
Rates of EHCP by ward have all increased from 2016 to 2019. Wards that have seen the biggest increase in rates are Stairfoot, Hoyland Milton, Penistone West and Dearne South.
Children living in Dearne South, Dearne North, St Helen’s and Stairfoot are the most likely to be receiving SEN Support (16.5%, 16.2%, 14.3% and 14% respectively) and are four of the wards with the highest proportion of deprived LSOAs. Those in Old Town, Cudworth and Dodworth are the least likely to receive SEN Support (6.6% 7% and 7.2% respectively).
As SEN support and EHCP represent differing levels of support for children with SEND it may be expected that those wards with the highest percentage of CYP with SEN support would also be those with the highest percentage of CYP with EHCP.
While this is true for some wards, for example St Helen’s is the highest ward for EHCP and 3rd highest for SEN Support, this is not repeated for many of the wards. Although the highest for SEN Support, the Dearne South ward is only the 9th highest level for EHCP. Conversely, Royston is the 2nd highest for EHCPs and 10th for SEN Support. Darton West is the 5th highest ward for EHCP yet is 16th highest for SEN Support. Both Royston and Darton West have no LSOAs in the 10% most deprived.
Comparing ward deprivation in terms of the percentage of children in poverty after housing costs to wards with highest percentage of children with SEN support shows quite a close correlation. But this is not the case when looking at wards with the highest percentage of EHCP, where there is no obvious relationship.
Nationally, children from low income families are more likely to be identified as having SEND however less likely to receive appropriate support or interventions that meet their needs. This is in part due to parents from deprived backgrounds having less agency to obtain support as a result of structural inequality. This can also result in them being less likely to receive support when seeking it. It is unclear if this inverse care picture is being replicated in Barnsley, however some of the local data would suggest this may be an issue. Further work is needed to understand the reasons for these disparities and whether all CYP with SEND are being supported appropriately.
Find out more about Barnsley's ward profiles.
The local strategic approach
Action planning
Barnsley’s local SEND Strategy 2020 to 2022 sets out the Local Area’s vision for children and young people who have special educational needs and/or disabilities, along with the priorities identified by leaders within the local area.
The vision articulates local area leaders’ commitment to:
- Enabling partnership opportunities with children, young people and parents/carers to develop services at an individual and strategic level.
- Developing and delivering a well-planned continuum of provision and integrated services which work closely with children, young people and their families to meet their needs at the right time and reduce reliance on specialist services.
- Supporting children and young people to live as ordinary a life as possible in their local community.
- Creating services, schools and settings which have the capacity and confidence to deliver high quality provision, which improves children and young people’s education, social and health outcomes.
The Barnsley Children Young People and Families’ Trust has identified SEND as a key priority for improvement. The Barnsley SEND improvement programme has five key priority areas:
- Priority 1: Early identification and support - We will work with early years settings, schools and universal health providers to get better at identifying and meeting children’s additional needs as early as possible.
- Priority 2: Education, health and care plans - We will improve planning process for EHCP.
- Priority 3: Participation and co-production - We will create more opportunities for children, young parents and carers to contribute to and co-produce strategies and planning for SEND Local Area arrangements.
- Priority 4: Specialist provision and services - We will develop specialist education provision locally so more children can be educated within Barnsley.
- Priority 5: Pathways to adulthood - We will develop better pathways to adulthood so that young people’s voice, needs and ambitions are the primary focus and they have access to timely and co-ordinated advice, support and service to enable them to plan for the future.
The SEND oversight board acts as the strategic driver for system changes to improve local area SEND arrangements. Undertaking this joint strategic needs assessment (JSNA) will provide us with a clearer picture of the underlying need of the population and suggest priority areas for improvement.
Lived experience of young people with SEND
Small qualitative focus groups and interviews have been conducted with local young people with experience of SEND by our Targeted Youth Support Service. Although not a representative sample, this data provides useful insight into some of the experiences of our SEND population (the full results are attached as an appendix).
Themes to emerge from the data were: education, respite, friendships and social activities, transition to adulthood, after education, employment and health and wellbeing.
Recommendations for improvement from the young people
The young people made a number of recommendations for each of the themes. They are as follows:
Education
- More needs to be done to tackle issues of bullying.
- More training on disability is needed for all school staff.
- Students should be taught about disability to develop empathy and understanding.
Respite
- Have different provision/ different activity offers in respite provision for young people with different needs and abilities.
Friendships and social activities
- Transport is a barrier to participation, sometimes the provision is there but young people cannot access it.
- Young people would like to be able to have more integration of SEND and mainstream groups, especially for those young people who do not necessarily identify as having a disability.
- Young people want to be able to access “normal” young person social activities with their friends.
- Need for more provision for older young people.
Transition to adulthood
- Most young people were not aware what transition to/preparation for adulthood is.
- They want more support in preparation for living alone, before the need to do it arises.
After education
- Young people worry about and want more preparation for when they need to live independently/without their parents.
- Young people worry about what they will be able to do when they cannot access youth provisions any more, many of them plan their weeks around the activities.
Employment
- Have more opportunities for work experience that has the potential to lead to employment.
- More training/support so that workplaces can support young people with SEND.
Health and wellbeing
- Better/ more consistent mental health support is needed.
- More specialist sexual health/education services are needed.
- More availability/flexibility of services such as TADS.
(Reproduced with kind permission from BMBC Targeted Youth Support).
A Life Course View
Maternal and birth factors
There are several different maternal and neonatal factors which influence the incidence of SEND. These include smoking, alcohol and drug use during pregnancy. A higher proportion of pregnant women in Barnsley are smoking at time of delivery compared to regional and national figures, 17% compared to 11% England, and 14% Yorkshire and the Humber. This has gradually fallen but did rise slightly last year.
Babies born at low birth weight or born premature have a higher prevalence of SEND Low birth rates for Barnsley are similar to national figures of around 3% of term babies.
Early years
The early years are critical for reducing health inequalities, ensuring good development, and have lifelong effects on health and wellbeing, educational attainment and economic status. Integrated children’s centres which combine education, care, family support and health service have most positive outcomes for children at low risk cognitive development and low social and behavioural difficulties.
All children are assessed at two years of age for their progress in eight different areas of learning and development. In Barnsley over half of children are below the expected stage of development for health and self-care, and speaking, and managing feelings and behaviour. Over a third are below expected for listening and attention and understanding. Just under a third are also below expected for making relationships. A greater proportion of boys are below expected levels of development, in particular for speaking, health and self-care and managing feeling and behaviour. In all aspects of learning and development, non-funded two year olds perform better than funded children. High quality early years provision is known to have a particularly positive effect for both children with SEND and children living in poverty. It is positive that 98% of early years settings in Barnsley are rated good or outstanding by Ofsted however they are being presented with increasingly complex children to manage.
Comparing recent data from early year’s assessments across Barnsley, it is clear that there are differences in the level of progress for some children. Overall, children living in Grimethorpe, Darfield South and Dearne perform less well than children from other areas.
Generally a higher proportion of girls are found to be at or above expected levels of development for most areas, this is similar to regionally and nationally. Girls in some areas locally perform worse than boys for managing feeling, speaking and health and self-care. Girls from some areas perform less well than boys in making relationships and self-confidence. There is a particularly high proportion of boys from the Dearne who are below expected for managing feelings and behaviour and a high proportion of boys who are below expected development for understanding in Grimethorpe and Darfield South. Three quarters of boys in Darfield South are below expected levels for speaking. It appears that some children are presenting to educational settings already behind at key milestones. The findings from the two year checks highlight the need for targeted work in certain areas for those families who need it most, to help them achieve equity with their peers in other areas.
Early years foundation stage
Last year 70% of children in Barnsley were assessed as achieving a good level of development at the end of reception, this is similar to the regional average and 1.5% below the England average and has increased slightly year on year.
All children are assessed against prime areas of learning, such as communication and language, and specific areas of learning, for example maths. Overall the percentage of Barnsley children achieving at least expected across all prime areas is the same as Yorkshire & the Humber and slightly below the national figures (78.6% compared to 79.4%).
Fewer Barnsley children were at the expected level of development for personal, social and emotional development compared to regional and national figures (83.5% compared to 85.2% England), the largest difference being for managing feelings and behaviour, which reflects the findings at the 2 year development check. Reading and mathematics performance were below national figures, over 4% more Barnsley children being below expected development for reading and over 3% below expected level for maths.
Overall the proportion of SEND children achieving the expected standard in all early learning goals was very similar to national figures with the SEND attainment gap being either the same or within a percentage point.
Educational outcomes
Pupils with SEND often experience poorer educational outcomes than pupils without SEND. The SEND attainment gap at KS1 for 2018/19 has improved compared to 2016/17. Figures for Barnsley are similar to those for England.
SEN attainment gap for KS2 is similar to the national picture and has not changed significantly since 2016/17. 89% of KS4 pupils with SEND are going to a sustained education, employment or training destination. This is in line with national figures.
School absence and exclusion
Pupils with SEND, particularly those from low income families are significantly more likely to be out of education either through exclusion or dropping out and subsequently are more likely to become NEET (Not in Education, Employment or Training). The relationship between SEND and poverty is interdependent with children in receipt of free school meals four times more likely than their peers to be excluded and those with SEND six times more likely to be excluded. Nationally, 75% of all permanently excluded pupils have some form of SEND identified. In addition, those young people attending the secondary schools in those most deprived areas, those from some minority ethnic backgrounds and those with experience of mental health concerns are also more likely to face exclusion.
The rate of fixed period exclusions has increased in mainstream schools however declined in special schools across England. It is thought the increase has been driven by the increase in exclusions in the North East region. After the North East, Yorkshire and the Humber is the second highest area for rates of fixed term exclusions (FTE)31. Nationally the exclusion rate across secondary schools (number of fixed term exclusions / number of registered pupils on roll in census day) is 10.13%, in Barnsley it is 46.4%. The national exclusion rate for those children on SEN Support is 15.10%, in Barnsley it is 118.7%. The national exclusion rate for children with an EHCP is 15.95%, in Barnsley it is 76.8%.
In May 16% of pupils with SEN support were persistently absent from school, 12% of those with EHCP. During the academic year 2017/18 children with SEN were twice as likely to be persistently absent than children without SEND, around 24% of pupils with EHCP were persistently absent compared to 11% of children without SEND and 20% of those with SEN support. These figures were worse than statistical neighbours and England figures although this is not as stark EHCP stats. Overall FTE are higher for Barnsley but considerably higher for pupils with SEND, 10.2% of pupils compared to only 6.2% England. Percentages are higher for both SEN support and EHCP pupils.
School placements
In 2018 mainstream education was the main educational provider for 40% of all pupils with an EHCP. 23% of these pupils were educated in special schools. 5.5% attended an independent special school, compared to 3.7% for England. 3.5% were educated elsewhere. A higher proportion of new EHCP pupils were attending mainstream school than England figures but nearly double the proportion were placed within independent special schools compared to national figures.
Of those pupils with an EHCP, 309 (13.9%) are in school placements outside of the borough. This is higher than the regional proportion of 6.2%. Barnsley has one of the highest proportions of ECHP pupils being educated outside of the borough of its statistical neighbours ranging from 3.5% to 14.1% (Teeside).
Approximately 10% of children and young people on the local authority’s electively home educated register have special educational needs.
Sufficiency is key outcome for the borough’s SEND Improvement Plan.
Mental health
Barnsley has a higher rate of SEMH as primary diagnosis for SEND than both the England average and that of its statistical neighbours, being the highest amongst statistical neighbours for primary school pupils and second highest for secondary school pupils. 3.06% of Barnsley school pupils have been identified as having SEMH needs; this is compared to the statistical neighbours’ and England average of 2.36% and 2.39% respectively.
When broken down by primary school, the figures are 2.7%, 2.2% and 2.2% respectively (Barnsley, Stat, England). When broken down by secondary school, the figures are 3.2%, 2.3% and 2.3% respectively (Barnsley, Stat, England). Barnsley’s rates for SEMH are significantly higher than that of statistical neighbours and England average and are the highest rates in the region.
Public Health England (PHE) using modelling estimate that 10.2% of children and young people aged 5-16 in Barnsley have a mental health disorder. This is compared to a 9.9% average across statistical neighbours and 9.2% England average. Using the same modelling techniques (ONS 2004 survey adjusted for socio-economic factors), PHE estimate 3.9% of children and young people aged 5-16 in Barnsley have an emotional disorder, which is in line with statistical neighbours. For hyperkinetic disorders, the figure is 1.7%, for conduct disorders 6.3%, which are similar to the statistical neighbours.
Another measure of mental and emotional health in the population is hospital admissions as a result of self-harm (10-24 year olds). Barnsley‘s rate of 695.2 admissions is significantly higher than the England average of 421.1 and third highest of the stat neighbours. Admissions appear to peak in the 15-19 age groups and this is where the largest gap between Barnsley and England (1155.1 vs 648.6 admissions) is. Subsequently there are large disparities within the borough. Central, Kingstone, St Helen’s and Stairfoot wards all have self-harm admission rates significantly higher than the Barnsley average. These wards also have some of the highest rates of pupils requiring SEN Support. Self-harm is an action on the local public health strategy.
National estimates suggest that between 1 in 10 and 4 in 10 children and young people experience mental health difficulties. Having SEN significantly increases the odds of having mental health difficulties ranging from 1.23-2.03 (Odds ratio) times as likely to experience these difficulties. Further work is warranted exploring the relationship between mental health and SEND in Barnsley.
Local Mental Health Pathways
A Designated Clinical Officer for SEND is a post that provides support on a range of health matters relating to the SEND population. Unfortunately for Barnsley, this post has been vacant for some time due to a failed recruitment. This has created a pressure in the system and has impacted on multi-agency working. Plans are in place for further recruitment to this post. If this subsequently fails, alternative strategies will be considered, including collaborating with neighbouring areas.
In the first quarter of 2019, Barnsley Child and Adolescent Mental Health Services (CAMHS) received 794 referrals. Of those, 377 did not require assessment or intervention (47.4%) of all referrals. The highest source of referrals not requiring assessment or intervention came from GPs (198 or 52%). The lowest source of inappropriate referrals came from self-referral (0.01%). It has to be noted that overall GPs were the largest referrers to CAMHS (318 or 40% of all referrals) whereas self-referral was the lowest referral source (10 or 0.01%). Referrals to CAMHS also came from Community and Hospital Paediatrics, Public Health Nursing, Social Care, Education and other hospital services.
Work is being conducted to improve the acceptance rate of referrals to CAMHS including education for referrers, parenting pathways and awareness raising campaigns.
Autistic Spectrum Condition
There are two pathways for Autistic Spectrum Condition (ASD) in Barnsley. One for those under 11 years of age and one for those over 11 years of age. The pathways were redesigned in 2015 and supported by a one off cash injection from Barnsley CCG to clear the backlog of cases on the waiting list, which was completed by December 2018. The under 11s pathway is currently managed by paediatricians at Barnsley Hospital NHS Foundation Hospital Trust (BHNFT). The over 11s pathway is managed by the CAMHS service run by South West Yorkshire Partnership Foundation Trust (SWYPFT). This pathway has been affected by staffing and capacity issues.
The waiting times for children on the under 11 pathway is between four and nine months (Oct 2019). The waiting time on the over 11 pathway as of July 2019 was 2.5 years (30 months). Long waiting times are particularly challenging for families who often feel “left in limbo” and this impacts on confidence in the wider SEND system. Further work has been done to develop the pathway for over 11s to reduce pressure in the system. It is too early to report progress on this.
Attention Deficit Hyperactive Disorder
Barnsley CCG are leading work to develop one neurodevelopmental pathway that will potentially have a pre-requisite that services will have undertaken an early help assessment on the family to ensure the most appropriate support is available at the earliest possible time. Early intervention is crucial to support families to build resilience, prevent problems from escalating and identifying inappropriate referrals which in turn helps to ease pressure on the system.
Family hubs are working with partners to provide early intervention to families on the ASC and ADHD pathway waiting lists. This work involves comprehensive assessment and action planning, one to one support and evidence based parenting in line with NICE guidance on ADHD. It is envisaged that for some families this support will be sufficient without the need for specialist mental health services. Initial feedback from Family hubs staff and families is positive however it is too early for a full evaluation.
Further vulnerabilities
Over 30% of children and young people in Barnsley with an EHCP are known to Children’s Social Care. This includes 385 (17.3%) as a child in need, 47 (12.2%) on a child protection plan, 53 (2.4%) as a looked after child and 17 (0.8%) as a care leaver. Of those with SEN Support needs, 474 (12.8%) are known as a child in need, 83 (2.2%) are on a child protection plan and 55 (1.5%) are looked after. Young people involved with social care are some of the most vulnerable however this combined with SEND enhances their vulnerability levels.
For those known to the Youth Justice Service 43 (1.9%) have an EHCP. For SEN Support this figure is 33 (0.9%). Anecdotal evidence from Barnsley Youth Justice Service reports that between 10-15% of the young people they work with have SEND. A learning disability nurse has been employed to screen all young people when they first enter the service. The service has also supported schools in triggering the EHCP process. Some of the issues that have been identified are: speech, language and communication; ASD, dyslexia, acquired brain injury and ADHD. The service also employs psychologically trained professionals in partnership with CAMHS to work with young people and is hoping to secure funding for a speech and language therapist.
Children in Barnsley with an EHCP were more likely to have additional vulnerabilities than those with SEN support. Over a third of pupils (35%) with an EHCP were in a family eligible for adult care services and just under a third received Early Help support services. This highlights a need to explore the generational impact of SEND but also identifying young people with SEND who are young carers and in a family that requires additional support. For SEN support just under a fifth had Early Help support services and 13% were children in need.
Support services
There are a number of sources of support provided which are brought together in one place, the Local Offer including: schools and colleges (specialist and mainstream, travel to school and college, childcare and education for the early years (0 to five years), health services including learning disability nurses, social care, training, housing, employment and leisure opportunities.
A few specific examples include:
- Early help assessment accessed through family hubs and ’I Know I Can’ young person centres.
- Group work delivered by Targeted Youth Support
- Public Health Nursing support
- Barnardo’s Young Carers
- DIAL Barnsley – offer advice and information to adults and children with disabilities and/or long term health problems
- Barnsley SENDIASS (SEND, information, advice and support service)
- KIDS: SEND participation and engagement in Barnsley – support parent forums and are a provider of young people’s participation
- Short breaks provision
- Barnsley CAMHS
- Barnsley Education Inclusion Services
Recommendations
The recommendations of this document have been aligned under similar headings as the local authorities SEND Improvement Plan. The aim of this is to align priorities in precise and consistent manner.
Priority 1: Early identification and support
Prevention
- The relationship between poverty and SEND is complex. Tackling childhood poverty and supporting low income families is central to improving outcomes and reducing demand.
- Access to quality early years provision is also protective and this should be encouraged, especially in those areas where EYFS attainment levels are poorest.
- Improved early identification (targeted) of families who need additional support to provide a supportive home learning environment would ensure less children present at early years settings behind in key milestones,
Life-course focus on SEMH
- Barnsley has high levels of SEMH as a primary diagnosis, particularly in secondary school. It has the highest proportion of SEMH in primary school compared to statistical neighbours. Poor early years outcomes for Personal, Social, Emotional Development may be contributing to higher levels of need in school aged children. Further work is required to explore the full reasons behind this.
- Children’s mental health and emotional resilience should be an area of focus. This should include early identification of families who need additional support to help prevent the development of SEMH need and implementation of evidence based interventions through the life course to improve outcomes. There should be further strategic alignment between SEND and mental health.
Early support and intervention for SEND
- CYP with SEND should be identified early and given quality support. Some of the data gathered suggests that improvements could be made in earlier identification for some of these children.
- Improvements in training and support to EYFS settings around SEND are in progress. The impact of this should be evaluated and reviewed with more training made available if necessary.
Priority 2: Education, health and care plans
Reducing inequalities
- Those children with the most need should receive the most support. There could be inequalities in access to EHCP provision across the borough. This should be further explored as to whether these inequalities exist and what could be done to overcome any barriers.
- Children and young people with SEND are significantly overly represented in exclusion figures in Barnsley. Young people being out of education and training perpetuates health and social inequalities. Work needs to be done with local schools to highlight the significance of this issue and engage partners with a workable solution for all parties.
Primary diagnosis and provision
- A higher proportion of Barnsley pupils have an EHCP compared to national figures. This is particularly true for those with a primary diagnosis of PD, SEMH and SLCN. The reasons behind this disparity should be investigated further to ensure children are being provided with the appropriate level of support.
Priority 3: Participation and co-production:
Working with CYP and families
- The system and how support is accessed needs to be accessible to parents, carers, young people and those involved in supporting these families.
- Children and young people had lots to say and plenty of suggestions about how things could be improved. Involving them in developing these ideas further and empowering them to be part of the improvement plan (eg as educators to peers, service providers and staff, meeting representatives) would help ensure services and support were fit for purpose and help them develop new skills.
- Carers reported that they were either unaware of the local offer or found it difficult to navigate or unhelpful. Co-producing the Local Offer and the web platform with CYP and Families would help ensure this was fit for purpose and matched the needs of CYP and their families. Information should be available in accessible formats and include clear process mapping so CYP and their families can better navigate the system.
Priority 4: Specialist provision and services:
Joint working
- SEND is a complex area, involving many different partners and organisations where outcomes are influenced by various factors. Whilst there has been good progress on improving the strategic oversight across stakeholders, further work at both strategic and operational level to strengthen working relationships, communication and coordination is important to get the best outcomes for CYP with SEND.
- Work is in progress to improve integrated working across social care and education and health to improve outcomes and service planning. This could perhaps be strengthened by providing a learning forum for all professionals supporting CYP and families to better understand each other’s role more clearly and support working relationships.
Records and case management:
- Good quality, reliable data and data sharing arrangements are important enablers for high quality, joined up care. Systems have been improved for tracking numbers and outcomes of integrated checks across 0-19 PNS, Early Years and SEND and a SEND vulnerability matrix is in development. Developing data sets that could follow cohorts of children through from two year health visiting development checks to leaving school could provide a rich picture of identification, progress and outcomes to guide further improvements in services.
- There should be strategic alignment between SEND and other relevant portfolios. SEND needs should be considered within other key policy areas.
Primary diagnosis and provision
- Barnsley is a clear outlier for MLD and SLD as primary diagnosis. The process for assessing primary diagnosis should be reviewed and if needed CYP with MLD reassessed to ensure that they have the appropriate support in place.
- The SEND support available in schools for these pupils is being strengthened through several different measures outlined in the improvement plan. The effectiveness of these should be evaluated and outcomes reviewed regularly to ensure the support is matching pupils needs.
Improve access and reduce waiting times
- The CAMHS service was out to tender at the time of writing. Work with commissioners and providers to develop processes to enhance pathways, direct appropriate cases to other areas of the system and support families at the earlies stage possible is needed.
- Waiting for long periods can significantly affect the situation families are in and place strain on the whole family. Work to reduce waiting times and improve access through evaluating the pathways, auditing referrals for appropriateness, utilising early help assessments and increasing capacity across the workforce is warranted as a priority.
SEND glossary
- ASD - Autistic Spectrum Disorder
- BME - Black and minority ethnic
- CYP - Children and young people
- EHCP - Education, Health and care plan
- FSM - Free school meals
- FTE - Fixed term exclusions
- IMD - Index of multiple deprivation
- JSNA - Joint strategic needs assessment
- KS - Key stage
- LSOA - Lower super output area
- MLD - Moderate learning disability
- NEET - Not in education, employment or training
- PD - Physical disability
- PSED - Personal, social and emotional development
- PHE - Public Health England
- SEMH - Social, emotional and mental health
- SEND - Special educational needs and disability
- SLCN - Speech, language and communication needs
- SLD - Specific learning difficulty
Additional resources
- The Children and Families Act
- The Equality Act
- Department for Work and Pensions. Family Resources Survey 2017/18
- Department for Education. Special educational needs in England
- Department for Education & Health. Special educational needs and disability code of practice: 0-25 years
- Department for Education. Special educational needs and disabilities: a guide for parents and carers
- Our borough profile
- Public Health England. Child and maternal health profiles
- Public Health England. Children and young people’s mental health and wellbeing profiles
- NICE Attention Deficit Quality Standard (QS39)
Social isolation
Why this is important
Loneliness is an increasingly important public health issue.Loneliness and social isolation can have a negative effect on our health, both mentally and physically. There are links between inequality and social isolation with many factors associated with this are unequally distributed in society.
Being cut off from social interaction is not only a problem for the elderly but also younger people, and the impact it has on our bodies is thought to be equivalent to smoking over a dozen cigarettes a day. Recent studies have shown that social isolation and loneliness are associated with a 50% excess risk of heart disease (Public Health England, 2015). Social isolation is the inadequate quality and quantity of social relations with other people at an individual, group and/ or community, whereas loneliness is an emotional perception that can be experienced by individuals regardless of the number of their social networks (Public Health England, 2015).
The Campaign to End Loneliness (2018) has described how loneliness and isolation can place individuals at a greater risk of cognitive decline and depression. People who experience loneliness are more likely to visit their GP, have a higher use of medication, higher incidence of falls and increased risk factors for long term care and chronic illness.
It is now possible to spend a day working, shopping or travelling without speaking to another human being and for some people this can be repeated day after day (HM Government, 2018). Our society is changing and we are experiencing a digital revolution which brings innovation, opportunities and possibilities to communicate and connect with others in ways that we have never seen before. However, we know that too many residents in Barnsley do not have the social connections they need or want.
The Barnsley picture and how we compare
-
In 2018/19, more than half (55.6%) of adult social care users (aged 18+) in Barnsley felt that they had as much social contact as they would like; significantly better than the England rate of 45.9% and the highest rate since 2010/11.
-
When compared to similar local authorities, Barnsley’s rate was the highest.
-
In terms of those aged over 65, a slightly higher proportion (56.1%) felt that they had as much social contact as they would like; again, significantly higher than the England rate of 43.5% and the highest of similar local authorities.
-
In respect of adult carers in Barnsley (aged 18+ and 65+), 32.6% and 37.1% (respectively) felt that they had as much social contact as they would like; similar to the England rates of 32.5% and 34.5%.
Link to data: PHE Productive Healthy Ageing Profile
What we're doing and the assets or services we have
The 2018 Director of Public Health Annual Report focussed on social connections and explored
how the world is changing and the importance of continuing to embrace digital and technological advances. The report contains examples of how individuals and organisations can improve our connections with others, plus it discusses how we need to change the way we connect with people in our communities.
All six Area Councils commission a social isolation service, commissioning different providers such as Age UK, B:Friend, Dial and the Royal Voluntary Service to provider slightly different services such as 121 befriending, emotional and practical support. Themes between the services include people aged 50 years plus, inventions within the home and skills and learning. Ward Alliances fund groups which provide activities that are not labelled as social isolation but are tackling the issue covertly. The Social Prescribing Service (commissioned by Barnsley CCG), is aligned to Area Council structures and supports resident’s wellbeing which includes, helping residents to engage with community activities, find work, training and volunteering opportunities.
Public Health is leading task and finish group which is exploring options for a borough wide approach to social isolation. Any strategy to prevent and tackle social isolation will link to other local and system developments and strategies such as: BMBC 2030, NHS Integrated Health and Wellbeing Teams and Primary Care Teams and Age Friendly Barnsley.
Opportunities for improvement or future development
The ‘Are you Contactless’ annual report contains the following recommendations for Barnsley;
- That we work with the Government to establish a clearer picture of the prevalence of loneliness through the development of a new national measure that we monitor locally and set a target to reduce.
- Ensure that the local social prescribing service, My Best Life, helps residents to connect with community support to restore social contact in their lives.
- That any evaluations from the many projects established to improve our connections with others within Area Councils are shared for future learning and to help build our local knowledge around what works.
- We will develop a local campaign which aims to reduce stigma and raise awareness of the importance of our connections with others, on our physical and mental health and wellbeing, for example it costs nothing to say ‘hello’.
- We will work with local employers to develop business champions who can tackle loneliness in the workplace.
- We will consider how tackling loneliness can be embedded in all our strategic plans and decision making through the Health and Wellbeing Board.
- Ensure that the Health and Wellbeing Board is fully sighted on loneliness locally and the steps we need to take to improve our connections.
- Step up our public health support to Area Councils commissions and grants.
- Develop the evidence-base around the impact of different initiatives in tackling loneliness, across all ages and within all communities.
Resources and supporting documents
Young people not in education, employment or training (NEET)
Why this is important
Engagement in learning and educational attainment is critical if young people are to make a success of their lives. Evidence shows that being not in education, employment or training (NEET) between the ages of 16 and 18 is a major predictor of later unemployment, low income, teenage motherhood, depression and poor physical and mental health. Young people who are NEET are at risk of not achieving their potential, economically or socially.
National research by York University suggests that there is a reasonable expectation that one in six young people who are NEET will never secure long-term employment, with the average individual lifetime public finance cost of a young person who is NEET at £56,300 equating to £12 billion across all young people who are NEET. The total associated loss to the economy, individuals and their families is just over £22 billion.
The Barnsley picture and how we compare
One of the key outcomes wanted for residents is that all are in education, employment or training at the end of compulsory education. Increasing the participation of Barnsley’s young people in learning and employment contributes to improved social mobility as well as stimulating economic growth.
To support more young people studying and gaining the skills and qualifications that lead to sustainable jobs and reduce the risk of them becoming NEET, legislation was included in 2013 to raise the participation age as contained within the Education and Skills Act 2008. This required that from 2013 all young people remain in some form of education or training until the end of the academic year in which they turn 17.
- The proportion of Barnsley’s 16 and 17 year old cohort who are NEET, or are Not Known (NK) in 2020 was 5.8%, similar to the England rate of 5.5%.
- Compared to similar authorities, Barnsley was ranked 3rd highest out of 16.
- Barnsley’s 2020 rate of 5.8% is the second highest since 2016 (6.8%).
What we're doing and the assets or services we have
Success in reducing the proportion of NEET 16/17 years olds has resulted from:
- Active caseload management and forensic tracking by the Targeted Information, Advice and Guidance Service (TIAG).
- Establishment of out-reach support in the heart of our communities to ‘take the service to young people’ thus improving access and support.
- Establishment of monthly ETE panels for some of our most vulnerable young people who are at risk of becoming NEET.
- Closer partnership working with key agencies and stakeholders.
- Revision of the data sharing agreement between providers and the council to ensure appropriate data about young people’s engagement is transferred in a timely fashion.
- A Progression Support Officer post being added to the TIAG team to provide ‘triage’ of young people whose current destination has not been confirmed. This has allowed the council’s support officers to focus capacity on supporting those we know to be NEET.
- Additional support for those who are at risk of becoming NEET through two projects – ESF Pathways to Progression and COVID Recovery Project.
- An extensive programme of support for schools and colleges to ensure they are delivering excellent careers guidance to ensure young people are supported to understand their options in order to make well-informed and realistic choices and thus avoid becoming NEET.
- Investment in two careers platforms – Start and Panjango.
- Two projects working direct with employers – ESF Business Education Alliance and the Careers and Enterprise Company funded Enterprise Adviser Network, to ensure young people understand and are prepared for the world of work.
Opportunities for improvement or future development
The recently extended European funded programme, Pathways to Progression, will continue to provide further capacity to work with those who are NEET and some way from the labour market. This programme also provides a small sum of funding for each participant to offer highly personalised support.
The More and Better Jobs Employer Promise is engaging increasing numbers of employers to offer of employability opportunities that can be incorporated into plans to support NEET young people.
A request has been put in to DWP to extend the current Business Education Alliance project which will enable us to continue to support small and medium sized enterprises to offer employability opportunities that will add to those forming the Employer Promise.
